Abstract
Abstract 757
Chronic lymphocytic leukemia (CLL) is the most common leukemia seen in adults. Previous population-based research in CLL has not represented the current ethnic makeup and diversity within the US population. We undertook a large Surveillance Epidemiology and End Results (SEER) based analysis to assess disparities in outcome among different ethnic subgroups of CLL patients, so that therapeutic resources can be utilized effectively.
The SEER-18 Registry (1973–2009) was used to retrieve a population of 60,293 patients with established diagnosis of CLL (Histology code: 9823). The cohort was restricted to adults (>18 yrs) diagnosed after January 1, 1992, since ethnic minorities were underrepresented in SEER prior to that. Cases reported in death certificate/autopsy, those without a confirmatory diagnosis, those with ethnicity recorded as unknown/other or those that did not have follow up post diagnosis were excluded. Using Cox proportional hazards models, adjusted for confounding variables, association between patient characteristics and survival (overall; OS and CLL-specific; CLLSS) was evaluated. Analysis was performed utilizing the SAS software (v9.2). All statistical tests were two-sided with a significance level of 5%.
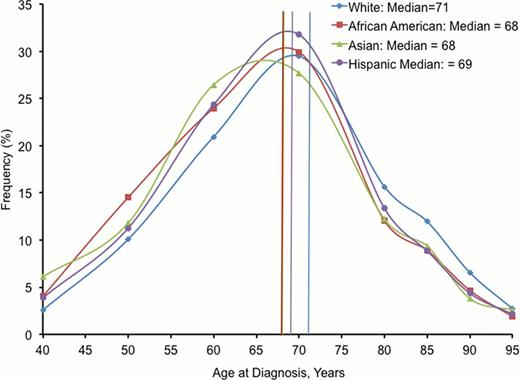
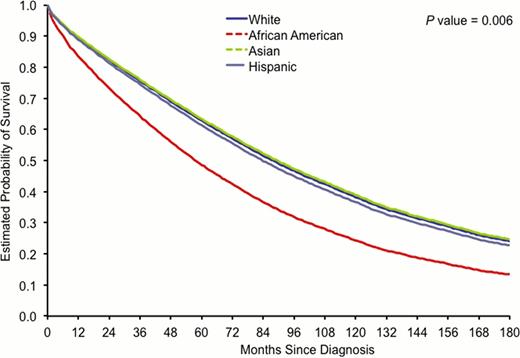
A total of 37,834 patients (22,581 males; 60%, 15,253 females; 40%) were included in the final analysis. Age group (yr) cohorts included: 18–44 (861; 2%) 45–54 (3,587; 9%), 55–64 (7,684; 20%), 65–74 (10,966; 29%), and ≥75 (14,736; 39%). For survival trends over time, stratification by year of diagnosis was used: 1992–1999 (9,837; 26%), 2000–2004 (14,129; 37%), 2005–2009 (13,868; 37%). Stratification by race/ethnicity included: White (32,980; 87%), African-American (AA: 2,486; 7%), Hispanic (1,536; 4%), Asian (737; 2%), and Native American (NA: 95; 0.25%). Median age ranged from 68 yr (AA and Asian) to 71 yr (Whites) (Figure 1). For survival analysis, NA ethnic group was excluded due to their small numbers. Females had a significantly better median OS (8.3 yr vs. 6.4 yr; p<0.001) as well as CLLSS (p<0.001) than males, when evaluated for the whole population and across different age groups. Both, OS and CLLSS progressively and significantly (p<0.001) declined with advancing age. Progressive significant improvement was seen in OS over time across cohorts by year of diagnosis (6.3 yr, 7.3 yr, 7.4 yr; p<0.001). This improvement in OS persisted over time for age groups <75 yr, but for ≥75 yr, the improvement was lost in the most recent time period cohort (2005–2009). The percentage of patients dying of CLL has decreased progressively over time suggesting an improvement in therapy. Among various ethnicities, Asians had the best (7.5 yr) and AA had the worst (4.8 yr) OS (p=0.006) (Figure 2) and CLLSS (p<0.001). In a multivariate model, AA continued to have the worst OS across all age groups (p<0.001), while Whites had the best OS in age groups <75 yr and Asians had the best among patients ≥75 yrs. Percentage of patients dying from CLL was highest in AA across age groups, but lowest for Whites in age groups <75 yr, while in Hispanics in patients ≥75 yr. Trends in CLLSS were noted to be more heterogeneous among ethnicities than trends in OS.
This report presents the largest population-based analysis of patient characteristics including ethnicity and survival in CLL in the era of novel therapeutic agents. Older patients had worse OS among all ethnic subgroups. Progressive improvement in CLLSS was noted over time suggesting a possible impact of new therapeutics, however this was not seen in ≥75 yr patients. AA patients had the worst OS among all ethnicities and age groups. This survival difference was most significant and pronounced in younger patients, which has important implications. For example, this survival disadvantage may represent poor access to optimal healthcare warranting development of new initiatives directed towards this ethnic minority. On the other hand discrete biological variants may underlie the more aggressive disease biology in younger AA patients underscoring the need to further investigate and delineate the molecular biology of CLL in ethnic minorities. Studies of outcome disparities are important not only for evaluating disease characteristics but also management needs of specific patient populations and are critical for designing programs to deliver optimal healthcare to ethnically diverse populations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal