Abstract
Abstract  700
700
Prognosis of lower (IPSS low/int-1) risk MDS is heterogeneous. Current prognostic systems rely on single time point cytopenia values (Hb level, ANC, PLT counts) at diagnosis (classical or revised IPSS [IPSS-R] Greenberg, Blood 2012) or during evolution (time-dependent IPSS/WPSS). Capturing the dynamics of continuous parameters can yield independent prognostic information as exemplified by lymphocyte time doubling in CLL. We analyzed the prognostic relevance of the kinetics of Hb, ANC and PLT in lower-risk MDS patients (pts) included in the prospective EUMDS registry.
Among the first 1000 pts included in the EUMDS registry, those fulfilling the following criteria were analyzed here: a) IPSS low/int-1; b) ≥3 visits (planned every 6 months) with ≥12 months follow-up; c) not treated with hypomethylating agents, G-CSF, hydroxyurea or lenalidomide. Dynamics of Hb, ANC, and PLT were studied by deriving linear models of each variable for each pt. Only pts with ≥3 measures of Hb, ANC and PLT and with stable or worsening corresponding cytopenia (model slope ≤0) were considered in each analysis, regardless of the goodness of fit (R2) of models. Time (T) to lose 1 g/dL of Hb (THb), 1.0 x109/L of ANC (TANC) and 50 x109/L of PLT (TPLT) were derived with the formula: T ∼ 1/slope. All survival analyses were made from the date of registry entry to last follow-up, death, or progression to AML. Unless specified, survival analyses were Cox models using continuous variables accounting for interactions.
530 pts met study inclusion criteria (M/F: 314/216, median age: 73y). WHO diagnosis was 5q- syndrome, RA, RARS, RCMD, RCMD-RS, RAEB-1 and MDS-U in 5, 21, 20, 38, 7, 8 and 2% respectively (resp). IPSS risk was low, int-1 and low/int-1 (cytogenetics not available) in 55%, 38% and 7% resp. At registry entry, median Hb, ANC and PLT were 10.4 g/dL, 2.4 x109/L and 187 x109/L resp. and 23% were RBC transfusion-dependent; 293 received an ESA. The median number of available blood counts was 4 (range 3–9).
THb, TANC and TPLT could be determined because of a stable or worsening cytopenia (slope ≤0) in 250/508, 258/495 and 301/509 pts with ≥3 values. There was no significant correlation between the number of values available and the goodness-of-fit (R2) of linear models (all P>0.3). Median THb TANC and TPLT were 23.5 (interquartile range [IQR]: 42.2), 28.7 (IQR: 52.1) and 26.9 (IQR: 49.2) months respectively. Because these figures are derived from linear models, they can be simply rescaled by a proportional extrapolation for daily practice (eg. −1 x109/L ANC at 28.7 months = −0.41 x109/L [12/28.7] at 12 months).
THb, TANC and TPLT were not correlated to age, cytogenetic risk, IPSS, IPSS-R or baseline simplified WPSS (Malcovati. Haematologica 2011; all P>0.2). TANC and TPLT (but not THb) were shorter in pts with baseline RBC transfusion dependence (P=.02 and .003, resp.).
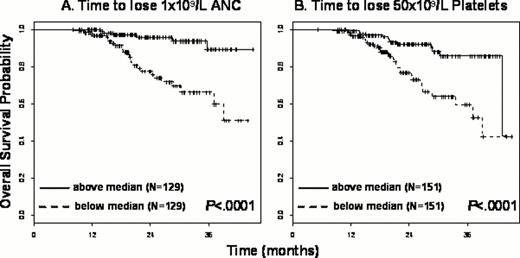
With a median follow-up of 20.9 months in the 530 pts, 19 patients have progressed (AML: 14, RAEB: 5) and 71 patients have died; 3-year estimates of overall (OS) and progression-free (PFS) survivals were 74.4% and 73.6%. All further analyses are shown for OS and give similar results for PFS. In univariate analysis, longer TANC (hazard ratio [HR] for 6-months increments: 0.88 [95% CI: 0.80–0.97], P=.008) and TPLT (HR: 0.01 [95% CI: 0.001–0.30], P=.007) but not THb (P=.07) were associated with prolonged OS. Pts with a ≥1 x109/L decrease in ANC in less than the median time of 28.7 months (N=129) had a 3-year OS of 66.3% [95% CI: 55.0–79.9%] vs 89.3% [79.7–100%]. Pts with a ≥50 x109/L decrease in PLT in less than the median of 26.9 months (N=151) had a 3-year OS of 59.4% [46.8–75.4%] vs 85.6% [77.5–94.6%] (Figure, both P<10−4). There was no significant difference in the cause of death between those subgroups. In multivariate analysis, the prognostic impact of TANC and TPLT remained independent of baseline IPSS (P=.006 and P=.01 resp.) or IPSS-R (both P=.01), and of simplified time-dependent WPSS (P=.004 and P=.03). A landmark analysis at 2 years, using only retrospective data to derive TANC and TPLT is planned.
In lower-risk MDS with stable or worsening cytopenias, kinetics of decline can be approximated to be linear to allow easy prognostic use in clinical practice. Faster decline of ANC and to a lesser extent of PLT counts, but not of Hb level (possibly because of transfusions and use of ESA), is associated with shorter OS and PFS, independently of IPSS, IPSS-R and WPSS.
Germing:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal