Abstract
Abstract 54
In early-stage Hodgkin Lymphoma (HL), treatment according to the early favorable or unfavorable subgroup is mostly guided by a staging system including the presence of certain risk factors. However, risk factors have grown historically, they differ between the various study groups worldwide, and some experts do not recognize the necessity for an early unfavorable group at all. To shed more light on this ongoing controversy, we analyzed the impact of risk factors used in different international staging systems on treatment outcome in early-stage HL.
In 1,173 qualified early-stage patients that were treated homogenously with 4 cycles of ABVD followed by involved-field radiotherapy within the GHSG trials HD10 and HD11, the impact of three international staging systems (GHSG, EORTC, NCCN) in discriminating early favorable and unfavorable treatment groups for progression free survival (PFS) and overall survival (OS) was assessed. Risk factors from the three definitions were tested for sensitivity and specificity for HL-related failure within 2.5 years, including only patients observed for at least 2.5 years (N=1,107). Univariate analyses of the respective single risk factors and of other known candidate risk factors as well as multivariate analyses were carried out using logistic regression, in order to evaluate the relevance and interaction of single factors.
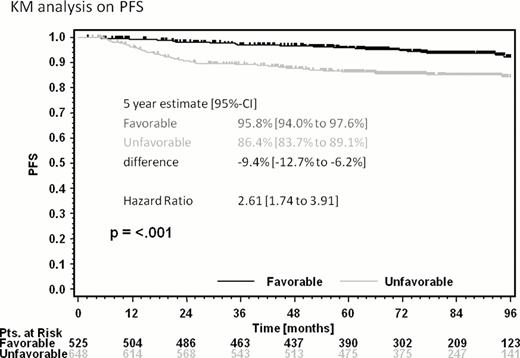
Median observation time was 80 months. Overall, 8% of early-stage patients had HL-related failure within 2.5 years. All three staging systems selected an unfavorable “high risk” group out of early-stage patients of comparable size (55%, 54%, and 56% of patients with the GHSG, EORTC, and NCCN system, respectively) with significant impact on PFS and OS. For example, with the GHSG system, PFS was 95.8% and 86.4% for the early favorable and unfavorable group at five years, with a significant difference of −9.4% (Figure 1).
Sensitivity for HL-related failure was high for all systems (84%, 79%, and 83%, respectively); however, there were high rates of false-positive results (1-specifity 54%, 53%, and 55%, respectively). Univariately, most analyzed factors had a relevant impact on the event rate. In multivariate analyses, the GHSG-system had 4/4, the EORTC-system 2/4, and the NCCN-system 3/5 independently significant risk factors. In general, models of high sensitivity included risk factors indicating large tumor burden and high tumor activity. Most risk factors for tumor-specific endpoints such as HL-related failure and PFS were also predictive for OS.
For the first time, the relevance of selecting an unfavorable risk group out of early-stage patients was proven in a large cohort of HL patients without treatment bias, with significant impact on PFS and OS. Thus, discriminating early favorable and unfavorable patients with HL by the identified risk factors is important in the modern combined modality treatment era and strongly recommended.
Progression free survival of early-stage HL patients undergoing 4 cycles of ABVD followed by IF-RT; favorable and unfavorable risk groups according to GHSG staging definition
Progression free survival of early-stage HL patients undergoing 4 cycles of ABVD followed by IF-RT; favorable and unfavorable risk groups according to GHSG staging definition
Engert:Millenium The Takeda Oncology Company: Honoraria. Borchmann:Millenium The Takeda Oncology Company: Research Funding; Takeda Pharma GmbH: Travel Grants, Travel Grants Other.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal