Abstract
Abstract 5154
Cytopenias following pediatric solid organ transplants (SOT) are common and often multifactorial. Rates of immune cytopenias (IC) are reported as high as 12. 2%. The aim of this study was to evaluate the demographics, response to treatments, and outcomes of a cohort of pts who developed IC following SOT at an academic pediatric center.
In this IRB approved, single center retrospective review, pts with ICs after SOT were identified by EMR search and transplant program databases. Pts with SOT from 1995–2012 and with laboratory and clinical evidence of autoimmune hemolytic anemia (AIHA), immune thrombocytopenia (ITP), or autoimmune neutropenia (neutimm) were included. “Severe” IC was defined as: ITP bleeding >grade 3 (Buchanan and Adix score); AIHA requiring >10 rbc transfusions; and neutimm with ANC <500 cells/mL. The data were collected using REDCap and analyzed in SAS 9. 4.
During a 17 year period, 2. 5% (19/752) of pts with SOT developed ICs. 68% (13/19) were male; median age at surgery varied by transplant type from 11 m in multivisceral (MV) pts to 27 m (kidney) (Table). Incidence varied widely by transplant type from 1. 2% (renal) to 23. 5% (multivisceral) (Table). Two of the 19 cases followed a second transplant; one pt received both liver and kidney transplants. AIHA (DAT+ for IgGand/or C3) was the most common IC (12/19, Table). Multiple cell lines were affected in 6 of 19 pts. Overall median time from transplant to IC was 8 m (range 3–46 m) and varied by transplant type from 3 m in liver to 74 m in heart. 2 transplant pts were ABO mismatched. 16/19 (84%) were on tacrolimus when the IC developed. Symptoms varied. 5/10 ITP pts had bleeding requiring therapy (i. e. > grade 3). In AIHA, median number of transfusions was 2. 5 (range: 0 to >40); only 2/12 AIHA pts had severe disease. All 3 neutimmpts were severe, and 2 developed serious bacterial infections. Most frequent treatments for IC included steroids (12/19), IVIG (12/19), and rituximab (6/19). The most effective therapies for AIHA were: switching from tacrolimus to sirolimus (100% response rate (RR)) and rituximab (75% RR). Switching off tacrolimus also gave the best ITP response rate (RR 100%), compared to IVIG (RR 50%) and steroids (RR 50%). For neutimm, tacrolimus to sirolimus switch had a 100% RR and IVIG (RR 50%). IVIG had only a 43% RR in AIHA, rituximab 0% RR in ITP, and steroids 50% RR or less in all three IC. Overall post-transplant immunosuppression was changed in 5 pts (26%); in all 5, tacrolimus was stopped. IC resolved in all 5 pts and did not recur when tacrolimus was restarted in 3 (median time off tacrolimus: 13 m). Median duration of follow up was 25 m (IQR 6–62 m) after diagnosis of IC. 17/19 pts were admitted to the hospital; 7 to the ICU related to IC. 1 pt developed PTLD prior to development of IC, and one after. 3/19 pts died; none were directly attributed to IC.
IC is not rare after solid organ transplant; incidence is very high post MV transplant. Time to presentation is variable. Pts with IC following SOT do not respond well to traditional first line therapies. However in this series, switching from tacrolimus to other agents resulted in remission of all affected cell lines in all five pts. Furthermore, pts switched back to tacrolimus did not redevelop IC. Temporary cessation of tacrolimus may help treat IC after SOT but must be weighed against the risk of organ rejection in this challenging clinical context.
Demographics, treatments, and outcomes of patients with immune cytopenias
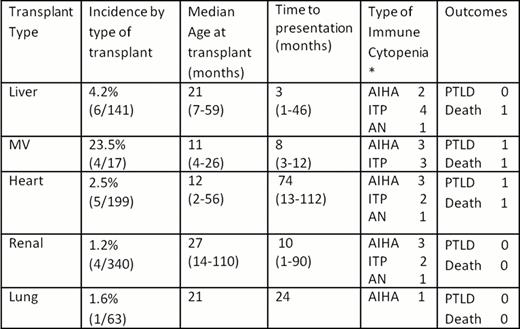
some pts with >1 immune cytopenia
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal