Abstract
Abstract 5073
Population based studies have reported that about 25–35% of DLBCL patients are older than 70 years. It is usually assumed that elderly patients are too frail to receive optimal chemotherapy regarding their frequent co-morbidities, leading to non-manageable treatment toxicity. However clinical trials dedicated to elderly patients demonstrated that a curative approach, based on a dose reduced anthracycline regimen combined with rituximab, is currently realistic in elderly patients. Nutritional parameters may be also crucial in the geriatric setting. Relationships between body compositions, specifically proportions of lean and fat tissues, with cancer incidence and cancer outcomes are of recent interest. In this field, sarcopenia, defined by the depletion of skeletal muscle, is known to be an unfavourable prognosis factor in patients with solid tumours. Its clinical relevance in NHL is still unknown. Taking advantage of the initial staging performed by computed tomography (CT) scan imaging to evaluate lean body mass, we assessed retrospectively the prevalence of sarcopenia and its prognosis value in a population of DLBCL patients older than 70 years treated by chemotherapy and rituximab.
This retrospective analysis included 82 patients diagnosed with DLBCL and treated by R-CHOP or R-miniCHOP.
Muscle mass was measured by analysis of stored CT images. A lumbar vertebral landmark (L3) was selected because skeletal muscle in this region corresponds to whole-body tissue quantities. To calculate tissue cross sectional area (cm2), the surface of the muscular tissues was selected according to CT Hounsfield unit. This value was normalized for stature to calculate the lumbar L3 skeletal muscle index (LSMI, in cm2/m2).
Sex-specific cut-offs for LSMI associated with mortality ascertained by optimum stratification were determined according to “R” for men and women (55. 8 cm2/m2 and 38. 9 cm2/m2 respectively).
Sarcopenia was determined in 82 DLBCL (median age: 78 y, range 70–95 y, 36 males; age adjusted IPI: 0–1 = 27, 2–3 = 55; mean body mass index (BMI) 24 kg/m2). According to the sex-specific cut-offs for LSMI, 45 DLBCL patients (55%, 24 males) were considered as sarcopenic. Sarcopenic patients, as compared to non sarcopenic patients displayed a similar level of aaIPI. By contrast the mean age was 80y in the sarcopenic group and 77y in the non sarcopenic group (p=0. 006).
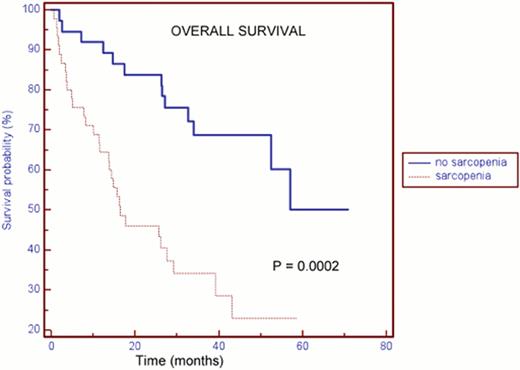
With a median follow-up of 39 months, the 2y overall survival in the sarcopenic population was 46% as compared to 84% in the non-sarcopenic group (HR = 0. 31; CI95%, 0. 16–0. 57; p=0. 0002). The prognostic value remains significant in the subgroup of patients younger than 80y (n=47) (HR=0. 2; CI95% 0. 07–0. 51; p=0. 0009). Mortality was mainly related to progressive disease in the sarcopenic group. Hypoalbuminemia is related to an unfavourable outcome (p=0. 002).
In multivariate analysis including albuminemia, age, treatment and aaIPI, sarcopenia remains predictive of the outcome (p=0. 03).
Our results indicate that refine anthropometric measurements based on lean or fat body composition, represent clearly a future field of investigation to optimize rituximab and cytotoxic drugs dose adaptation in a geriatric context.
The LSMI, evaluated by routine staging CT scan is a relevant and predictive tool in elderly DLCBL treated by rituximab plus chemotherapy. Sarcopenia defined by this index is related to albuminemia and age but remains predictive of the outcome independently of the aaIPI. A prospective multicentric study is currently on-going to confirm these results and to integrate this anthropometric measurement in a larger comprehensive geriatric assessment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal