Abstract
Abstract  484
484
Treatment options for individuals diagnosed with iron deficiency anemia (IDA) include oral or intravenous iron. Oral iron may not increase patient hemoglobin levels adequately, due to poor compliance and/or suboptimal gastrointestinal absorption due to inflammation-mediated induction of hepcidin, which regulates iron homeostasis. This study evaluated whether hepcidin levels can be used to identify patients with IDA who are unresponsive to oral iron therapy.
Hepcidin levels were assessed in a subset of subjects enrolled in a randomized trial comparing oral iron (ferrous sulfate) to intravenous iron (Injectafer®[ferric carboxymaltose, FCM]) in subjects with IDA (Hemoglobin [Hb] ≤ 11 g/dL; and ferritin ≤ 100 ng/mL, or ≤ 300 ng/mL when transferrin saturation (TSAT) was ≤ 30%) (Szczech et al Amer Soc Nephrol 2011; 22:405A). Subjects who met the inclusion criteria underwent a 14-day (run-in) course of ferrous sulfate 325 mg, three times per day. Subjects with an increase in Hb ≥ 1 g/dL were considered to be “responders” and not randomized. “Non-responders” were randomized to ferric carboxymaltose (2 injections of 750 mg given on Day 0 [day of randomization] and Day 7) or oral iron for 14 more days. Hb levels and markers of iron status were assessed at screening (day-15), day-1 and day 35. Hepcidin levels were analyzed at screening (Day -15) in an initial Cohort (I) of 44 patients, 22 responders and 22 non-responders. A hepcidin value of >20 ng/mL was identified for further analysis for predictive values for non-responsiveness to 14 day oral iron run-in in 240 patients (Cohort II). Hepcidin levels were also analyzed at Day -1 and Day 35 in a Cohort (III) of patients who were then randomized to FCM vs. oral iron therapy.
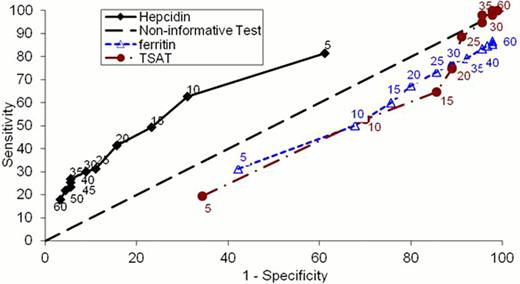
Hepcidin screening levels in Cohort I were significantly higher in the non-responders vs. responders (33.2 vs. 8.7 ng/mL, p < 0.004). Twenty one of 22 non-responders had hepcidin values > 20 ng/mL. For Cohort II, mean hepcidin levels were again significantly higher in the non-responders vs. responders (38.4 vs. 11.3 ng/mL, p = 0.0002). Utilizing a hepcidin criterion of > 20 ng/mL, we found a sensitivity of 41.3% (26 of 150), specificity of 84.4% (76 of 90), and a positive predictive value (PPV) of 81.6% (62 of 76) for non-responsiveness to oral iron (Figure: The Receiver Operator Characteristic curves present plots of sensitivity vs. (1-specificity) for hepcidin, ferritin, and TSAT at the various cutoff levels indicated near the respective curves in the same color as the respective curves). While ferritin < 30ng/mL or TSAT <15% had greater sensitivity (77.3% and 64.7%, respectively), their PPVs (59.2% and 55%) were inferior to PPVs for hepcidin. Patients subsequently randomized to FCM vs. oral iron responded with Hgb increases of ≥1 g/dL for 65.3% vs. 20.8% (p <0.0001)and mean Hgb increases of 1.7 ± 1.3 vs. 0.6 ± 0.9 g/dL (p = 0.0025), respectively.
Our analysis provides evidence that non-responsiveness to oral iron in patients with iron deficiency anemia can be predicted from patients' baseline hepcidin levels, which have superior positive predictive values compared to transferrin saturation or ferritin levels. Furthermore, non-response to oral iron therapy does not rule out iron deficiency, since two thirds of these non-responders to oral iron responded to IV iron.
Goodnough:Luitpold: Consultancy. Off Label Use: ferric carboxymaltose for treatment of iron deficiency anemia. Morris:Luitpold: Consultancy. Koch:Luitpold: Employment. He:Luitpold: Employment. Bregman:Luitpold: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal