Abstract
Abstract 4715
Allogeneic hematopoietic stem cell transplantation (HCT) represents potential curative option for patients with high risk hematological malignancy. However, HCT is still associated with high treatment related mortality (TRM). Extensive research in graft vs. host disease (GVHD) prevention and treatment of relapse post-transplant is being done to improve HCT outcomes. Although the transplant center experience and transplant volume has been correlated with improved outcomes after allogeneic HCT, the effect of physician's experience and continuity of care on outcomes after HCT in hematological malignancies is not known. We hypothesized that continuity of care along with physician experience would improve outcomes after HCT. Retrospectively, we reviewed the survival outcomes of 28 consecutive patients with high risk malignancy that underwent HCT from July 2010 to May 2012. A single 9 years experienced physician followed up those patients both as inpatient and outpatient from the time of initial consult up to last follow. The average percentage of care provided by the transplant physician to the 28 patients was 84% of the total billing visits.
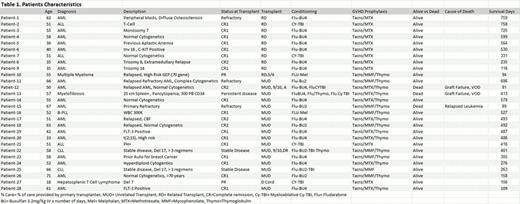
Patients characteristics including age, diagnosis, disease risk, status at HCT, donor source, conditioning regimen, GVHD prophylaxis and survival status are shown in table 1. All the patients received an established conditioning regimens and standard GVHD prophylaxis according to the donor source (table 1).
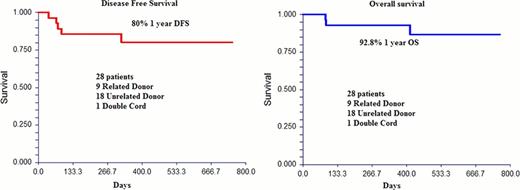
Median age at transplant was 53 y/o. Donor source was 9 related donors (RD), 18 MUD donors and 1 double cord blood. All patients engrafted except two patients. One graft failure was in a patient who received a marrow product with low CD34 count. The other graft failure was in a myelofibrosis patient who failed to engraft after 3 attempts. With median duration of follow up of 422 days; at one year the overall survival (OS) was 92.8% (C.I. 83%–100%) and disease free survival (DFS) was 80% (C.I. 64%–96%). The cumulative incidence of acute GVHD was 52.5%, 55% for RD and 51% for MUD. Only 2/28 patients developed grade III and IV acute graft vs. host disease (Both MUD). Surprisingly, the cumulative incidence of chronic graft vs. host disease was higher for RD compared to MUD, 100% vs. 64%, respectively (P=0.1). Overall cumulative incidence of chronic GVHD was 74%. Both cumulative incidence of relapse and TRM were low of 7% at 1 year post transplant.
Continuity of care when combined with the physician experience may result in superior survival outcomes in patients with high risk malignancy undergoing allogeneic HCT. Despite the small sample size, this intervention resulted in unexpected improved survival rate with lower TRM and relapse rate. Design of future prospective studies to address the impact of continuity of care and physician experience on outcomes after HCT is needed.
Khaled:Celgene and Takeda Pharmacutical: Honoraria, Speakers Bureau. Solh:Celgene: Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal