Abstract
Abstract 4501
CMV (Cytomegalovirus) reactivations are a major cause of morbidity and mortality in recipients of hematopoietic cell transplantation (HCT). Risk factors for CMV reactivations have not been fully elucidated. We evaluated first and subsequent CMV reactivations.
Three hundred and forty seven patients transplanted consecutively between year 2005 and 2010 at Princess Margaret Hospital were assessed. CMV monitoring was performed by pp65 antigenemia testing. Positive patients (defined as >1 positive cells per 105 peripheral blood leukocytes examined) were treated preemptively with ganciclovir.
206(59%) patients received HCTs from related and 141(41%) from unrelated donors. 152(44%) were female and 195(56%) male. Graft versus host disease (GVHD) prophylaxis included Cyclosporine (CSA)/Mycophenolate mofetil (MMF) (n=100, 28.8%), CSA/Methotrexate (MTX) (n=101, 29.1%), CSA/CAMPATH (n=139, 40%), other (n=7, 2%).
With a median follow up of 15 months, 132 patients (38%) had at least one CMV reactivation. 67(51%) were Recipient (R) +/Donor (D) +, 61(46%) R+/D- and 4(3%) R-/D+. The median time to first reactivation was 35.5 days with a range from 13 – 1052 days.
Risk factors for the occurrence of the first CMV reactivation were analyzed using death and relapse as competing risk factors. Older age at transplant (p-value 0.0375), female gender of recipients (p-value-0.0193) and presence of GVHD (p-value-0.0002) were significant factors for first CMV reactivations by univariate analysis. Conditioning regimens (p-value- 0.3294), donor type (p-value 0.1769) and lymphocyte count on the day of reactivation (p-value- 0.2308) were not significantly associated with first CMV reactivation. GVHD prophylaxis showed a trend (p-value- 0.0587). Multivariate analysis confirmed older age at transplant (p-value- 0.0258, odds ratio 1.024, 95%CI [1.003–1.045]), female gender of recipient (p-value- 0.0123, odds ratio 1.838, 95%CI [1.141–2.959]), GVHD prophylaxis with alemtuzumab (p-value 0.0324, odds ratio 2.121, 95%CI [1.148–3.917]) and presence of GVHD (p-value- <0.0001), odds ratio 2.935, 95%CI [1.754–4.910]) as independent variables.
The time to first CMV reactivation was shorter in patients with GVHD prophylaxis using alemtuzumab containing regimens (34 days vs 60 days for CSA + MTX and 105 days for CSA + MMF, p= 0.0241), with low lymphocyte counts (<0.75 × 109/L, 42 days vs 112 days, p=0.0015), and presence of GVHD (40 days vs 79 days, p= 0.05).
A number of patients experienced second or multiple CMV reactivations (Table 1) with a maximum of 10 reactivations. The median time to a subsequent reactivation from previous was 44 (range 35–127) days.
| # Reactivations . | n (%) . | Median time from HCT to reactivation in days (range) . |
|---|---|---|
| 1 | 132 (100) | 35.5 (13–1052) |
| 2 | 75 (57) | 77 (41–1638) |
| 3 | 41 (31) | 116 (59–334) |
| >3 | 21 (16) | 154 (90–1034) |
| # Reactivations . | n (%) . | Median time from HCT to reactivation in days (range) . |
|---|---|---|
| 1 | 132 (100) | 35.5 (13–1052) |
| 2 | 75 (57) | 77 (41–1638) |
| 3 | 41 (31) | 116 (59–334) |
| >3 | 21 (16) | 154 (90–1034) |
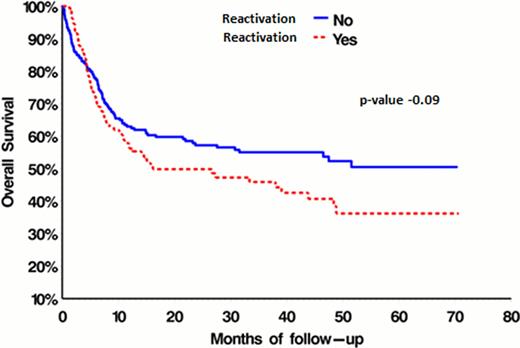
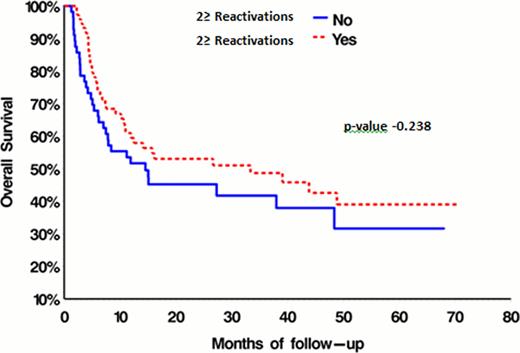
The overall survival of patients that have not reactivated (Fig. 1) was not significantly different from that of patients with either 1 or multiple CMV reactivations (Fig. 2).
Age at transplant, female gender of recipients, GVHD prophylaxis and presence of GVHD were identified as risk factors for the first CMV reactivation. The time to first reactivation was influenced by GVHD prophylaxis, lymphocyte count and presence of GVHD. Overall survival was not affected by CMV reactivations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal