Abstract
Abstract 4485
Allogeneic stem-cell transplantation (ASCT) is curative for many malignant and nonmalignant hematological disorders. Limitations of expanding this form of treatment are related primarily to non-relapse mortality (NRM) associated with reconstituting the recipient's immune system. We aimed to study reconstitution of lymphocyte subsets after matched and mismatched transplantation.
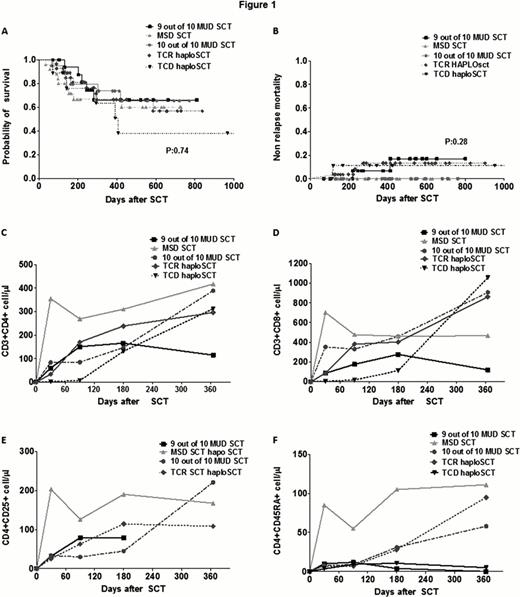
Lymphocyte subsets (absolute numbers of CD3, CD4, CD8, CD19, CD56, CD25, CD45RA, CD45RO) were evaluated by flow cytometry at 1,3,6 and 12 months (mo) post-ASCT. Lymphocyte recovery was determined using means at each time point and group differences were assessed using analysis of variance. Kaplan-Meier survival curves were used to estimate time-to-event outcome measures and the log-rank test was used to evaluate differences between groups. 100 patients (pts) were included in the study. 25 pts received a matched sibling donor transplant (MSD), 20 pts a 10/10 MUD, 18 pts a 9/10 MUD, 9 pts a T cell depleted haploidentical (TCD haplo), and 28 a T cell replete haploidentical donor (TCR haplo). 53 pts received bone marrow and 47 had peripheral blood stem cells. Most patients were treated for acute leukemia (AML 41, ALL 23), 16 MDS, 6 CML, 4 CLL, 5 lymphoma. Median age was 43 years (range: 20–71). The median follow-up was 13.6 mo. 60 pts were alive and disease-free at last follow-up and 28 pts died 75% due to relapse. Non-relapse mortality (NRM) was 6% for the entire cohort.
Overall, alive pts (vs who died) had higher mean CD3 (615 vs 349, p=0.03 on day 90), CD8 (427 vs 187, p=0.03 on day 90), CD4 (391 vs 54, p=0.01, on day 365) cells, and lower mean CD56 cells (178 vs 300, p=0.01, on day 30) post ASCT. Pts who progressed (vs did not), had lower 1 year mean CD4 cells (123 vs 394, p=0.02), lower mean CD3 cells (359 vs 1147, p=0.06), with no differences in CD8, NK, and CD45RA. NRM was associated with higher mean NK numbers at 6 months (499 vs 188, p=0.01) and with lower mean CD3 at day 90 (184 vs 557, p=0.07). T-cell recovery occurred most rapidly in MSD transplants (Figure1C), and compared with 10/10 MUD had higher mean CD3 cells in the first mo (1085 vs 510, p=0.01), CD4 in the first 6 mo (310 vs 147, p<0.01 day 180) and CD4CD45RA in the first 6 mo (105 vs 31, p=0.02 on day 180). Interestingly, we have found that higher CD4CD25 cell numbers recovered early and most rapidly in the MSD transplants, which may partly explain a lower incidence of GVHD in this group. Overall, TCR haplos had a similar pattern of T-cell recovery and outcomes as 10/10 MUDs (Figure1C-E). There was a significant delay in CD3 recovery between MSD and TCR haplos in the first 3 mo (mean 779 vs 483, p=0.04 on day 90), CD4 (mean 270 vs 170, p=0.03 day 90) and in the first 6 months for CD45RA (mean 105 vs 28, p=0.01 on day 180), while these differences were significant only at day 30 for CD8 cells (mean 703 vs 88, p<0.01). No significant differences in T cell subsets were found between 10/10 MUD and TCR HaploSCT for CD3, CD4, CD8, CD45RA and CD4CD25 for any time points. Of all types of transplant, TCD haplos had most impaired T-cell reconstitution and worst outcomes (Figure 1A and 1B). As previously reported it was characterized by rapid early NK cell recovery and delayed CD3, CD4, CD8 reconstitution. Interestingly, pts surviving 6–9 months post-transplant recovered CD3, C4, CD8 cells; however, naïve T-cell recovery remained impaired for more than 1 year post-transplant, suggesting that T cell recovery comes predominantly from the memory T cell compartment.
In conclusion, these results suggest that recovery of lymphocyte subsets may vary widely with the type of transplant, may correlate with outcomes, and it is important to be further explored in this setting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal