Abstract
Abstract 448
POEMS syndrome is a rare form of plasma cell dyscrasia that presents with polyneuropathy and various other systemic findings. Patients with 1–3 lesions and bone marrows without clonal plasma cells have been given targeted radiation as the initial and potentially definitive therapy. Outcomes of patients treated thus have not been systematically studied.
One hundred and forty-six patients with POEMS syndrome were seen at the Mayo Clinic in Rochester, MN between January 1999 and September 2011. Charts of patients with research authorization were reviewed with IRB approval. Patients who had been given targeted radiation as their initial primary therapy were eligible for this study. Thirty-eight patients satisfied criteria and comprise the study population. Three patients had either short or poorly documented follow-up and were excluded from the response and time to next treatment analyses. Patients were categorized by systems that were involved at diagnosis, time of radiation, response after radiation, and the need for further therapy. Statistical analyses were performed using JMP statistical software (SAS, Carey, NC).
The median age was 50, with 76% of the population being male. Median time from diagnosis to radiation was 0.7 months, ranging from 0 to 9.4 months. 20, 14, 11 and 2 patients had immunosuppressive therapy with corticosteroids, IVIG, plasmapheresis, or rituximab, respectively, directed at a prior presumptive, but incorrect, diagnosis of CIDP. Five patients had one cycle or less of alkylator, lenalidomide, or bortezomib, prior to receiving what was hoped to be definitive radiation therapy. The median number of bone lesions was 1, range 1–6. In total 55 lesions of the possible 64 were irradiated being mostly found in the pelvic bones including the sacrum, ileum, ischium, and pubis. The median dose of radiation given was 45 Gy range 35 Gy to 54 Gy.
Forty-nine percent had clinical improvement, 26% had a mixed clinical picture, 3% merely stabilized, and 23% had a clinical worsening. 29% had a complete hematologic response, 9% had a very good partial hematologic response, 9% had a partial hematologic response, 26% had no hematologic response, and the remaining were either non- or oligo-secretory or undocumented. 11% had a complete FDG-PET response, 11% had a partial FDG-PET response, 11% had no FDG-PET response, and the remaining had no documented FDG-PETs to analyze. 11% had a complete VEGF response, 3% had partial VEGF response, 14% had no VEGF response, and the rest were either not documented or unevaluable.
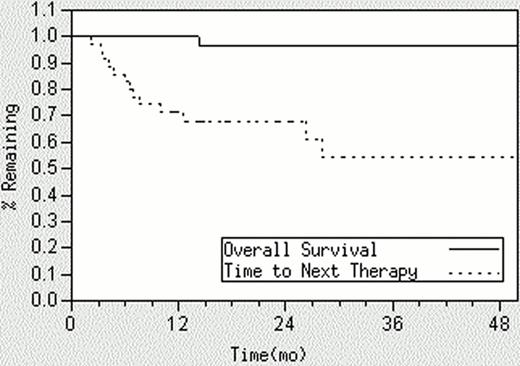
The median follow up of living patients is 30 months, and the 4-year OS is 95%. Forty-eight percent of patients went on to receive additional therapy after their radiation (Figure ). The median time to next therapy (TTNT) for these patients was 7.6 months (range 2.2 –73 months). Subsequent therapies included high dose chemotherapy with autologous hematopoietic stem cell transplant (n=10), low dose alkylator (n=2), thalidomide/lenalidomide (n=3), and more radiation (n=3). None of the baseline characteristics predicted for whether a patient would receive (or require) subsequent therapy, including the number of bone lesions at baseline.
The results show that radiation is sufficient to produce clinical improvements and hematologic and radiographic responses approximately 50% of patients, even those with as many as 3 lesions.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal