Abstract
Abstract 4388
Hemophilia is caused by a single-gene defect in which a small increase in gene products could transform a severe form of hemophilia into a mild one. Hemophilia treatments are readily available in developed countries, however In Egypt, Most hemophilia patients are treated with plasma or cryoprecipitate, where the treatment is associated with a high risk of blood-borne diseases. Liver transplantation in human and canine hemophilia A results in an increase in factor VIII levels to normal. Studies showed that BMCs not only differentiated into hepatic and liver cells, but they did express the intact gene of the FVIII A3 domain.
In this work we studied the ability of bone marrow derived stem cells from hemophilia patients' relatives (carrier or normal) to be differentiated into hepatocytes expressing FVIII m-RNA in vitro as a step towards transplantation in haemophilia patients. It was necessary to prove that the applied culture conditions were successful not only to obtain hepaotocyte morphology but also hepatocyte ability to produce FVIII.
The study was conducted on family relatives of five hemophilia A patients attending the hematology clinic, Cairo University hospitals. From each family, one hemophilia A carrier and one healthy person were subjected to the study. Informed consent was obtained from the participants. BM-HSCs were cultured in liquid culture containing HGF for 6 days. Differentiation into hepatocytes was evaluated by alpha-fetoprotein (AFP) expression using immunohistochemistry, albumin synthesis in culture supernatant using microalbumin assay kit, factor VIII activity by one stage clotting assay and expression of FVIII mRNA by RT-PCR.
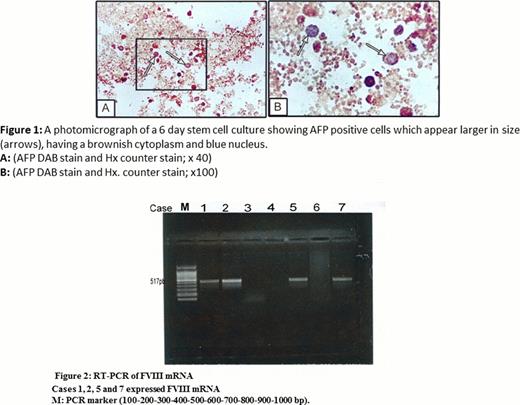
Cell morphology changed after 6 days culture; round or polygonal-shaped cells with moderate cytoplasm and a medium-sized nucleus were observed. Morphologic confirmation of hepatocyte differentiation was done by immunocytochemistry; human alpha fetoprotein positive cells were detected in the culture. The positive cells appeared round or pear shaped, most of them contained one nucleus. However, few cells were binucleated with brown stained cytoplasm and bluish nuclei (Figure 1 A, B). By image analysis, the mean number of alpha fetoprotein positive cells estimated in10 random high power fields was 11 ± 1.6, 11 ±1.8 cells/HPF in the carriers and controls respectively. Immunophenotyping after culture; the percentage of CD 34+ve cells for the carrier group ranged from 0.5 to 2.5 with the mean of 1.2 ± 0.8 and from 0.7 to 2.1 with the mean of 1.5 ± 0.7 for the control group. There was no statistically significant difference between the two groups (p > 0.05) and the percentage of CD 90+ve cells for the carrier group ranged from 11.1 to 14.2 with the mean of 12.7 ± 1.2 and from 12.6 to 13.8 with the mean of 13.3 ± 0.6 for the control group. There was no statistically significant difference between the two groups (p > 0.05). On comparison between immunophenotyping before and after culture in both groups, statistical analysis showed highly significant decrease in CD34 positivity (p value 0.002 and 0.001) in the carriers and controls respectively associated with highly significant increase in the percentage of CD90 positive cells (p value 0.000) in the two groups. Albumin secretion was detected in the culture supernate at the 6th day culture, the mean albumin level was 0.52 mg/L ± 0.32 and 0.6 mg/L ± 0.4 in the carriers and controls respectively. F VIII activity was estimated; with the mean of 0.14%±0.021% and 0.5%±0.4% in the carriers and controls respectively. Transcription of FVIII m-RNA was detected by qualitative RT-PCR in 2 carriers and all controls (Figure 2).
BM derived hepatocytes showed positive AFP expression. Functional tests performed showed their ability to produce albumin and perform FVIII activity. Also FVIII mRNA expression was detected. Induction of HSCs differentiation by in vitro manipulation may become a valuable tool to provide a cell source for liver transplant procedures and treatment of haemophilia patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal