Abstract
Abstract 4292
Acute lymphoblastic leukaemia (ALL) is the most common type of childhood cancer in East Asian, Caucasians and in the United States. Previous studies have shown poorer survival from childhood ALL among Asian compared to Caucasian populations. The US National Cancer Institute's Surveillance, Epidemiology and End Results program from 1998 to 2008 showed that poorer prognosis waseven observed in East Asian children living in the United States, compared to non-Hispanic Whites. This finding is interesting in that Asian ethnic groups are not socioeconomically disadvantaged in the United States relative to non-Hispanic whites as shown by US Census data.
The primary goal of this study was to compare the outcome of Belgian and Vietnamese children with ALL, treated with the same protocol (French acute lymphoblastic leukemia protocol FRALLE).
The Belgian series included 107 patients (aged less than 19 at diagnosis) followed at Cliniquesuniversitaires Saint-Luc (UCL), Brussels, Belgium between 2001 and 2011. The Vietnamese series included 166 patients from Blood Transfusion and Hematology Hospital, University of Medicine Pham Ngoc Thach (UPNT) at Ho Chi Minh city, Vietnam (aged less than 16 at diagnosis) and followed between 2005 and 2011. Clinical andbiologicalvariables and survival rates were compared using Cox Proportional Hazards Regression model. The association between clinicaland biological variables and both adverse drug reactions and relapse free survival were analyzed using Log-Binomial Regression model. All statistical analysis was performed using the ‘Epi’ and the ‘Survival’ package of the R 2.15.0 software.
The two populations were comparable regarding age at diagnosis, sex ratio, initialwhite blood cell count, cytogenetic and steroid responsiveness at day 8. A higher prevalence of L2 type-ALL according to the FAB classification was found in Vietnamese children (81.3 % L2 in Vietnam vs 44.9% in Belgium).
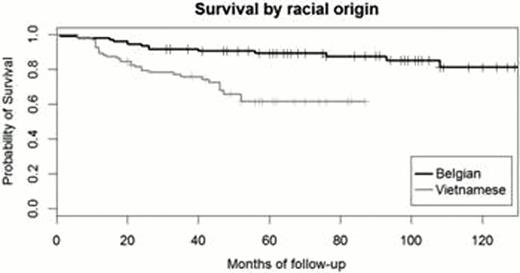
Vietnamese patients had a significantly lower survival than Belgian patients (p<0.001) (figure 1). In the multivariate analysis model, relative risk of death for Vietnamese children was 2.61 (95% CI= 1.03–6.65) (p = 0.04).
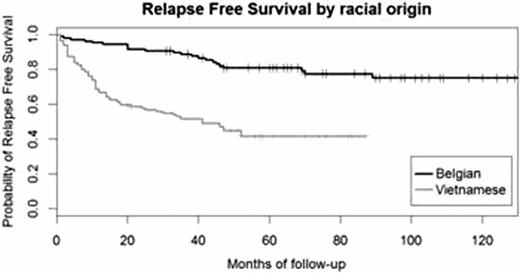
Compared to the Belgian cohort, Vietnamese children had a lower relapse free survival (figure 2) and a higher relativerisk of relapse of 3.01 (95% CI = 1.53–5.93). They also disclosed a higher incidence of methotrexate-related grade 3 or 4 side effects (36.2% vs 5.6%).
Compared to Caucasians treated with the same protocol, a poorer overall survival was confirmed in children with ALL treated in Vietnam. Relapse free survival was lower and adverse reaction rate higher among Vietnamese children. Racial differences in pharmacogenetics of drugs as well as additional factors such as social status, lack of antibiotic prophylaxis or delayed access to care due to remoteness may explain these observations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal