Abstract
Abstract 4203
The major drawback of HLA-haploidentical stem cell transplantation is graft-versus-host disease (GVHD): however, the GVHD can be overcome using substantial T cell depletion method (Perugia), the use of a high dose ATG (Beijing), or the posttransplantation cyclophophamide method (Johns Hopkins). These transplant procedures are found to be effective for the achievement of donor engraftment and immunological tolerance: however, graft-versus-leukemia (GVL) effects are not enough strong to prevent disease relapse. To harness GVL effect of HLA-haploidentical grafts, our regimen for unmanipulated haploidentical myeloablative transplantation is designed for GVH reaction to remain to some extent in the short time after transplantation using a small dose of ATG 2 mg/kg, coupled with GVHD prophylaxis containing a low dose of steroid (methylprednisolone 1 mg/kg). We hypothesize that allogeneic immunological response by donor T cells under low cytokine milieu exerts potent GVL effect without GVHD. This regimen was applied to patients with hematologic disease in an extremely high risk.
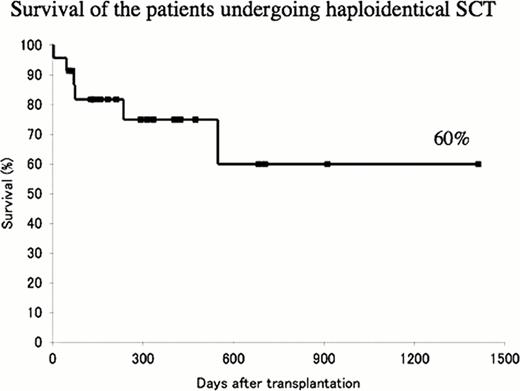
From August 2008 to June 2012, 23 patients with high-risk or refractory hematologic diseases underwent unmanipulated peripheral blood stem cells using a graft from HLA-haploidentical related donor (11 cases were HLA 2 antigen-mismatched and 12 HLA 3 antigen-mismatched in the GVH direction). Patients' characteristics are sex: male 11, female 12, age: 17–46 years old (median 34), disease: AML/MDS 7, ALL 10, ML 5, others 1. All patients except for 5 underwent transplantation in non-complete remission (non-CR) status, including 5 patients in induction failure, and 10 in resistant relapse. Eleven patients with leukemia who underwent in non-CR state had a median of 66% blasts in the bone marrow (range, 10.6 – 97.0 %). Patients received a conditioning treatment consisting of fuludarabine, cytarabine, cyclophsphamide, TBI 8Gy and ATG (thymoglobuline) 2 mg/kg. GVHD prophylaxis consisted of tacrolimus and methylprednisolone (1 mg/kg). One patient dies of pneumonia on day 3. Among 22 patients that could be evaluated, the engraftment rate was 95.5% (one patient had graft rejection because of donor-specific HLA antibody). Neutrophil (>0.5×109/l) and platelet (>20×109/l) engraftment was achieved on day 11 and on day 32, respectively. All patients who underwent transplantation in non-CR achieved CR after transplantation. Eleven patients (52.4%) had no GVHD. Nine patients (42.9%) developed grade II-III acute GVHD. One patient died of cardiac failure on day 46, 1 VOD on day 74, and 1 GVHD on day 235. Two patients died of relapse on days 70 and 548. Four of the 8 patients with leukemia who had more than 50% blasts in the bone marrow at the time of transplantation survive in CR. The overall survival is 60% at 3 years (Figure 1).
Our regimen for HLA-haploidentical transplantation using a small dose of ATG coupled with low dose of steroid exerts a strong GVL effect even for patients who had chemorefractory disease, and transplantation-related toxicities, including GVHD, are acceptable. As a result, patients, of whom the majority had a high tumor burden, achieved a high rate of long-term survival. Thus, our strategy for haploidentical stem cell transplantation is promising, although our results will have to be confirmed in a large-scale study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal