Abstract
Abstract 4169
Mycophenolate mofetil (MMF) has emerged as a potential substitute to methotrexate in patients given calcineurin inhibitors for the prophylaxis of GVHD prior to allogeneic hematopoietic cell transplantation. However, a comprehensive literature evaluation of MMF vs. methotrexate is lacking.
This study aims to compare the efficacy and safety of MMF vs. methotrexate as part of the GVHD prophylaxis regimen in patients given allografts.
Systematic review and meta-analysis of all comparative trials of patients given allografts and administered GVHD prophylaxis with a regimen containing MMF or methotrexate. Electronic search was conducted until June 2012. Primary outcome was acute GVHD. Secondary outcomes were all-cause mortality, relapse rate, non-relapse mortality, chronic GVHD, rate of mucositis, and the time to neutrophil and platelet engraftment. For dichotomous data, relative risks (RR) with 95% confidence intervals (CIs) were estimated and pooled. For continuous variables we calculated weighted mean difference (WMD).
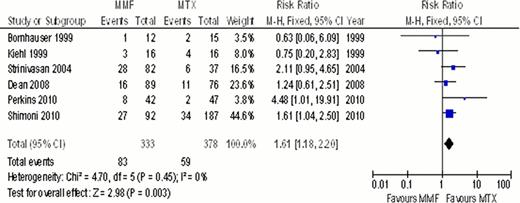
Our search yielded 11 trials, 3 were randomized control trials (RCTs) and 8 were either one arm intervention trials compared to historical controls or retrospective studies. There was no difference in the overall incidence of acute GVHD (RR 1.06; 95% CI 0.93–1.21, 11 trials) with similar results in a sensitivity analysis including only RCTs. Conversely, incidence of grade 3–4 acute GVHD was higher in patients given MMF (RR 1.61; 95% CI 1.18–2.20, 6 trials, Figure). However, this association was no longer statistically significant when only patients given allografts from matched siblings or those given myloablative conditioning were analyzed (RR 1.56; 95% CI 0.95–2.55, 5 trials and RR 1.40; 95% CI 0.82–2.39, 4 trials). All cause mortality, non relapse mortality, relapse rate and the incidence of chronic GVHD were comparable between the two groups. Incidence of mucositis was significantly lower in patients given MMF (RR 0.35; 95% CI 0.25–0.49, 8 trials) and the time to neutrophil and platelet engraftment was shorter in the MMF arm (WMD (−4.05); 95% CI (−6.17) – (−1.3), 6 trials and WMD (−3.74); 95% CI (−6.3) – (−1.18), 4 trials, respectively).
MMF, compared to methotrexate, given as GVHD prophylaxis is associated with reduced transplantation associated toxicities, however with increased severity of acute GVHD. Further RCTs to identify the subgroups of patients who will benefit the most from MMF are warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal