Abstract
Abstract  4094
4094
Telomeres are linear DNA structures at the ends of chromosomes that help to maintain genome stability. In the absence of effective telomere-protecting mechanisms, chromosomes lose a few base pairs (bp) of their telomeric DNA at each mitotic division and thus telomere length (TL) is also considered a marker of cell aging. In the hematopoietic system, TL of both early and committed progenitors progressively shortens with age, as in other highly replicating tissues. Moreover, many studies demonstrated that high proliferative stresses, including bone marrow (BM) regeneration after transplantation, cause a non-physiological TL shortening. Indeed, recent studies suggest that post-autograft TL correlates with TL of grafted material (Ruella et al, 2010). In order to address this issue, TL has been evaluated in a series of adult subjects engrafted with umbilical cord blood (UCB), a graft source characterized by cells harboring very long telomeres. Aim of the study was to verify whether despite the high replicative stress during engraftment, UCB hematopoietic stem cells may renew the recipient BM, maintaining the biologic characteristics of the graft.
TL was evaluated on peripheral blood (PB) cells from 20 adult recipients of umbilical cord blood transplant (UCBT). They had been transplanted due to acute leukemia (n=12), multiple myeloma (n=2), non-Hodgkin's Lymphoma (n=3) or chronic myeloproliferative disease (=3). TL analysis was performed in absence of signs of the previous disease and at complete hematological recovery, at a median of 9 mos. (range 1–73) since UCBT. At TL analysis, cell blood counts revealed median values of 7,540 white blood cells/μL (range 2,870-18,800), 11.9 gr% of hemoglobin (range 8.3–14), and 144,000 platelets/μL (range 41,000–351,000). TL was evaluated on both whole PB cells and separated cell populations, i.e. MNC and granulocytes, obtained following Ficoll gradient cell separation. TL was also determined on a series of 47 UCB samples, including samples from cord blood units employed as graft material for four patients of the present series. TL was determined on DNA extracts by Southern blot analysis, according to well established procedures. Briefly, DNA fragments were separated by agarose gel electrophoresis. The Telomere Length Assay Kit (Roche Diagnostic) was used for the hybridization phase and for each telomere smear, mean terminal restriction fragment (TRF) lengths and the point of maximum signal intensity defining the highest concentration of telomere repeats were calculated using Quantity One software (Bio-Rad Laboratories, UK).
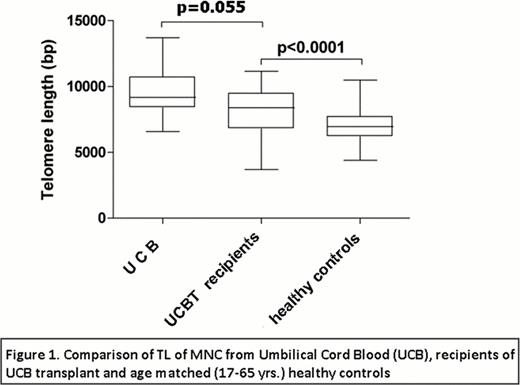
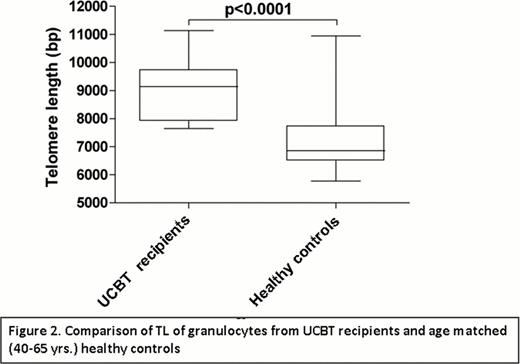
Overall, TL in PB cells following UCBT showed a rapid fall compared to TL values that characterize cord blood cells. In our series of 47 UCB samples, the median TL-TRF on MNC is 9,171 bp (range 6,573-13,695), whereas MNC from our UCBT recipients showed a median TL-TRF of 8,689 bp (range 5,982-11,149) (p=0,055). When values were distributed according to the age of UCBT recipients, TL remained higher than TL obtained from a large series of hundreds of normal control subjects. Indeed, median TL-TRF on MNC from healthy controls is 6,951 bp (range 4,375-10,467), significantly shorter compared to MNC from UCBT recipients, as shown in Figure 1. Similar results were obtained when TL was assessed on whole PB cells and on separated granulocytes. In fact, the most marked difference in TL between UCBT recipients and normal controls was observed on granulocytes. This was particularly clear among subjects aged >40 yrs. As shown in Figure 2, median TL-TRF on granulocytes from UCBT recipients aged 40–65 yrs. was 9,138 bp (range 7,644 – 11,138) compared to 6,857 bp (range 5,773 – 10,946) of granulocytes from age-matched normal controls. Overall, PB cells from subjects grafted with UCB showed a TL slightly longer than in the youngest control population of 0–20 yrs. of age. Lastly, no difference in TL was observed according to time elapsed since transplant, with analogous TL values in subjects evaluated at less or more than 6 months since UCBT.
The results indicate that despite the high replicative stress during BM engraftment, UCBT regenerate a hematopoietic system characterized by long TL. This suggests that in the transplant setting the use of young donor cells such as UCB may replace patient BM with not only a healthy but also a biologically young hematopoietic system.
Rambaldi:Hoffman-La Roche: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal