Abstract
Abstract 3987
Autologous stem cell transplantation (ASCT) is the gold standard as first-line treatment in young patients with multiple myeloma (MM). Prognostic factors have been usually related to patient characteristic and disease stage. Few investigations on the pattern of relapse or progression after ASCT have been addressed. The differentiation of serological or asymptomatic progression versus clinical relapse requiring treatment is also an important issue. The aim of this study was to investigate the characteristics at the time of relapse or progression in patients with MM who received ASCT as part of a first-line treatment.
Two-hundred and eleven patients underwent melphalan-based ASCT at our institution during the last 18 years. Of these, 170 patients (87M/83F; median age 56 years, range 25 to 70) who achieved at the least a minimal response (PR) after no more of two induction lines before ASCT are the basis of this study. Initial baseline demographics, clinical and laboratory data at relapse or progression, and information concerning treatment and follow up were collected. The M-protein heavy-chain isotype was IgG (57%), IgA (23%), light chain only (14%) and others (3.5%). Only 2.5% were oligosecretory MM. Extramedullary plasmacytomas (EMP) were observed in 37 out of 170 patients (22%) at diagnosis. The ISS stage was I (45.3%), II (26.5%), III (18.8%) and unknown (9.5%). 12.6% of the patients had a serum creatinine level ≥2 mg/dL and 16.2% had hypercalcemia. The median follow-up for alive patients was 3.9 years (range 4 months to 18 years). Response, relapse, and progression were defined according to European Blood and Marrow Transplantation (EBMT) criteria.
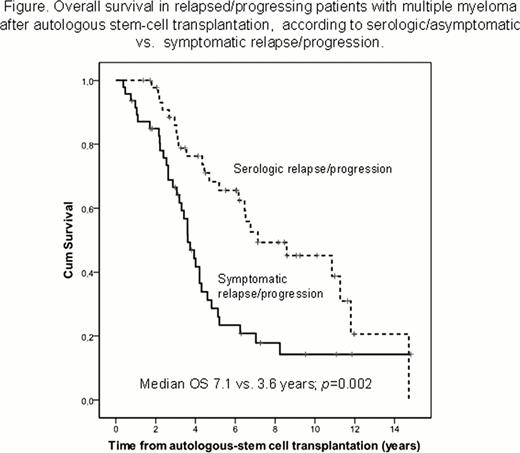
Median PFS was 3.3 years (CI 95% 2.7 to 3.9 years) and the median OS of 6.8 years (CI 95% 3.9 to 9.6 years). 47.7% of the patients achieved a complete remission (CR). As of December 2011, 93 patients (54.7%) had relapsed or progressed after ASCT. 37 out of the 93 patients (40%) had relapsed from CR, while the remaining 60% had progressed from PR. A serological or asymptomatic relapse/progression was as frequent as a symptomatic one (49.5% vs. 50.5%, respectively), the latter requiring immediate treatment in the median of a month. Patients with serological relapse/progression had a significantly longer OS than those requiring immediate treatment (p=0.002)(Figure). The main clinical reasons to start myeloma therapy were anemia (43%), new bone lytic lesions (36%), EMP (23.7%), bone pain (14.4%), renal insufficiency (12.2%) and/or hypercalcemia (9%).
22 of the 93 patients (24%) relapsed/progressing patients had EMP at the time of progression. In three of them, the extramedullary involvement was the only criteria of progression. The presence of EMP at diagnosis was significantly associated with extramedullary disease at relapse (p=0.001). In fact, 12 out of the 22 patients (54.5%) with EMP at relapse had also EMP at the time of diagnosis.
Median time between serological relapse or progression and treatment was of only 5.6 months (range 0 to 5.6 years). However, in 12 out of 46 patients (26%) with serological relapse/progression, treatment was not initiated within first two years. Finally, time to next treatment was significantly longer in patients relapsing from CR (median 2.85 years; CI 95% 2.1 to 3.6) vs. those progressing from PR (median 1.65 years; CI 95% 1.1 to 2.2) (p=0.017).
After ASCT, serological or asymptomatic relapse/progression is observed in about one half of the patients. The treatment-free interval in these patients is longer in patients relapsing from CR than in those progressing from PR. Patients with symptomatic relapse/progression have shorter OS. Extramedullary involvement is frequent, being the highest risk in patients with EMP at diagnosis. Finally, relapse/progression with extramedullary disease only is rare.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal