Abstract
Abstract 3948
Multiple myeloma (MM) is characterized by the production of a monoclonal immunoglobulin of constant isotype and light chain restriction due to the clonal proliferation of neoplastic plasma cells. The optimal treatment in patients younger than 65 years includes induction therapy followed by high- dose therapy/autologous stem-cell transplantation (ASCT). On the other hand, the emergence of oligoclonal bands is a benign phenomenon frequently associated with complete remission (CR) after ASCT. The aim of the present study was to investigate the incidence, biological characteristics, duration and prognostic value of the oligoclonal bands in patients with MM who underwent ASCT at our institution in the last 18 years.
Two-hundred and eleven patients underwent melphalan-based ASCT at our institution from March 31st, 1994, to December 27th, 2011. Of these, 199 patients (109M/90F; median age 55 years, range 25 to 70) who achieved at the least a partial response (PR) after ASCT are the basis of this study. Initial baseline demographics, clinical and laboratory data, and information concerning treatment and follow up were collected. No patient was lost to follow-up. The median follow-up for alive patients was 4.7 years (range 4 months to 18 years). A retrospective systematic review of all serum and urine immunofixation (IFE) studies was carried out. An oligoclonal humoral response was defined as the presence of a serum and/or urine IFE monoclonal spike different from the original myeloma protein either in heavy and/or light chains, as well as at IFE migration pattern. Response, relapse, and progression were defined according to European Blood and Marrow Transplantation (EBMT) criteria.
Median PFS was 87 out of the 199 patients (43.7%) achieved CR. The median progression-free survival (PFS) and overall survival (OS) after ASCT were 3.2 and 6.6 years, respectively. Oligoclonal bands were observed in 34% of the patients, but with different prevalence according to the use of novel agents vs. conventional chemotherapy (63% vs. 22%; p=0.0001) in induction. This phenomena was almost exclusive of patients in CR compared to other degrees of response (92% vs. 8%; p=0.0001). Five patients with IgA and five with Bence Jones MM were the only ones being in PR and having a very transient coexistence of the original M-protein with IgG oligoclonal bands in serum. The median number of different isotypes accounting for oligoclonal humoral response was 2 (range 1 to 6) and this phenomena lasted for a median of 1.35 years. Serum bands were more frequent (75.4%) than those in urine and the main involved serum heavy-chain was IgG (73%), with almost the same distribution kappa/lambda. Kappa light-chain was the predominant isotype in urine (60%).
In the overall series, all the oligoclonal bands disappeared before serological and clinical progression, except in two settings. First, patients (n=6) who progressed with extramedullary disease with soft-tissue plasmacytomas without significant bone marrow or serological involvement, had persistent oligoclonal bands for several months. Second, patients with Bence Jones MM (n=6), showing urine M-protein progression at the time of relapse had also a transient persistence of serum oligoclonal bands.
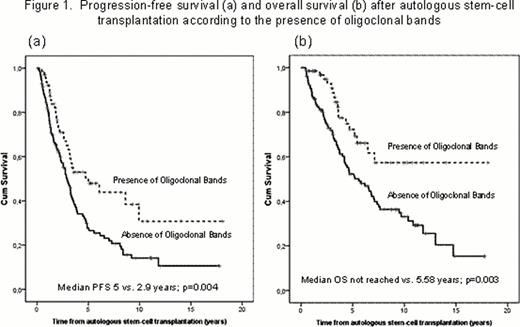
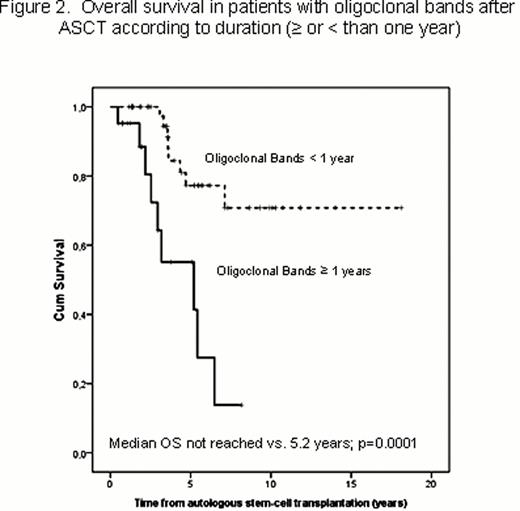
The presence of oligoclonal bands after ASCT resulted in a significantly longer PFS (p=0.004). This translated in a significantly longer OS in patients with this humoral oligoclonal response (median OS not reached vs. 5.58 years; p=0.003) (Figure 1). An oligoclonal humoral response stable more than one year after ASCT was associated with a significantly longer clinical PFS and OS than those with shorter duration (p=0.008 and p=0.0001, respectively). Of note, the estimated survival of patients with oligoclonal bands lasting for more than one year at 10 years is 70% (Figure 2). In contrast, the PFS ad OS of patients with oligoclonal bands lasting for less than one year were similar to those who never developed this phenomena.
The emergence of oligoclonal bands after ASCT is a prognostic factor and it is usually observed in patients in CR. They reflect a robust humoral immune response and consequently an immune system reconstitution. Duration of this humoral response is also associated with a significant survival prolongation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal