Abstract
Abstract 391
Traditionally, the focus of VTE diagnostic is on deep vein thrombosis (DVT) of the leg and pulmonary embolism. Until recently, upper extremity DVT (UEDVT) was regarded as an uncommon and relatively benign presentation of venous thromboembolism; however, the more widespread use of central venous catheters has caused a significant increase in its incidence. Moreover, recent data indicate that 10–25% of these patients may have pulmonary embolism. Therefore, effective and safe diagnostic strategies are needed. The use of an algorithm combining a clinical decision score, D-dimer and ultrasonography is well-established for suspected lower limb DVT, but has not been evaluated in suspected UEDVT. This diagnostic management study assessed the safety and feasibility of a new diagnostic algorithm in patients with clinically suspected UEDVT.
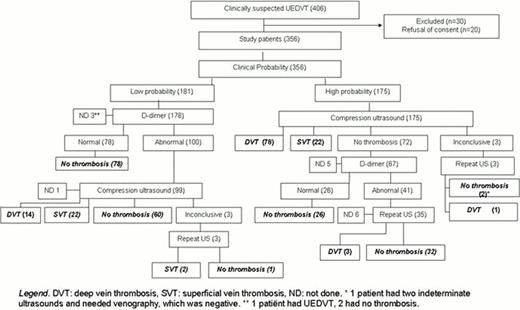
In- and outpatients with suspected UEDVT were recruited from January 2010 until July 2012 in 17 hospitals in Europe and the United States. To confirm an acceptable failure rate of excluding UEDVT (upper 95% confidence interval below 3%), approximately 400 patients needed to be included. Main exclusion criteria were previous UEDVT and the use of therapeutic doses of anticoagulants. Informed consent was obtained from all participants. The algorithm consisted of the sequential application of the Constans' clinical decision score (Constans et al, Thromb Haemost 2008), D-dimer testing and compression ultrasonography. Patients were first categorized as UEDVT likely or unlikely by the Constans' score. In the patients with an unlikely score and a normal D-dimer, UEDVT was considered excluded and no further testing was done. All other patients underwent compression ultrasonography, which first assessed the deep veins for the presence of UEDVT and then the superficial veins for the presence of superficial vein thrombosis (SVT). Ultrasonography was repeated in case of an indeterminate ultrasonography result, or in patients with a high probability score, abnormal D-dimer and a normal ultrasonography. The primary outcome was the 3-month incidence of symptomatic UEDVT and pulmonary embolism in patients with a diagnostic work-up excluding both UEDVT and SVT.
The study population comprised of 356 consecutive patients with suspected UEDVT. The algorithm was feasible and completed in 96% (Figure). Of the 356 patients, 181 had a low probability score and D-dimer was measured. In 78 patients (22%) a normal D-dimer combined with a low probability score excluded UEDVT without any imaging, and these patients all had an uneventful 3 month follow up. An abnormal D-dimer test result was found in 100 patients, who underwent ultrasonography. In 3 patients, D-dimer measurement was not done, and these patients received ultrasonography right away. Of all patients with a low probability score, 15 patients had UEDVT, 24 patients had SVT, while thrombosis (both deep and superficial) was excluded in 141 patients. One remaining patient died of progressive cancer before ultrasonography could be done. All 175 patients with a high probability score underwent compression ultrasonography right away, which was repeated if indicated. Of these patients with a high probability score, 82 had UEDVT and 22 had SVT. In 71 patients, thrombosis was excluded, including 11 patients in whom the protocol was not followed completely. To summarize, of the 356 included patients, 97 patients had UEDVT (27%), 46 had SVT (13%) and in 212 patients the algorithm excluded UEDVT and SVT (60%). Of all patients in whom the algorithm excluded UEDVT and SVT, one patient developed UEDVT during follow-up for an overall failure rate of 0.47% (95%CI: 0.0–2.6%). Final results of the definitive study population of 407 patients will be presented.
A new diagnostic algorithm which combines a clinical decision score, D-dimer and ultrasonography can safely and effectively exclude venous thrombosis of the upper extremity. This approach is attractive as it is simple, quick and non-invasive, and very similar to the well established algorithm for suspected DVT of the leg which could facilitate its implementation in clinical practice.
Flow-chart of the study
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal