Abstract
Abstract 3830
The EUMDS registry was established to obtain an overview in the real world MDS demographics, diagnostics and disease-management. From April 2008 until December 2010, 1000 newly diagnosed patients with IPSS low and int-1 risk MDS were included in 14 countries and 118 participating centers. The major clinical problems in MDS are the consequences of cytopenias and disease-progression. Therefore, the most important treatment goals are improvement of cytopenias and prevention of leukemia.
To describe the causes of early mortality and to analyze the outcome of the first 1000 patients in the registry with and without disease-progression at 24 months follow-up.
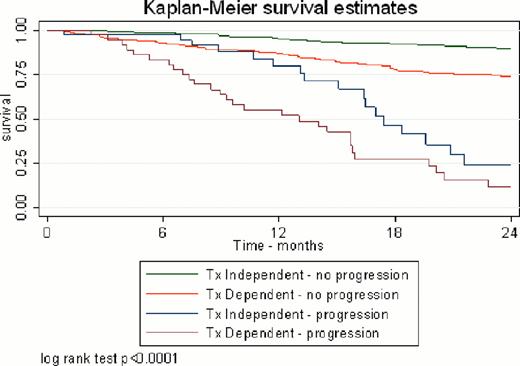
The median age of the population was 74 years (range 18–95), 60% were male. The most frequent co-morbidities were hypertension (46%), diabetes mellitus (18%), arrhythmias (12%), and thyroid diseases (12%). The WHO subgroups are RCMD (39%), RA (19%), RARS (17%), RAEB-1 (13%), RCMD-RS (7%), MDS-U (3%), and del5q (2%). IPSS score (n=935) was 0 in 48%, 0.5 in 31% and 1 in 14% of the patients. WPSS score (n=924) was Very Low in 32%, Low in 38%, Intermediate in 19% and High in 4% of the patients (Table1). 184 of 1000 patients (18%) had started MDS specific treatment within 3 months after diagnosis: this increased to 43% at 24 months of follow-up. 15% of the patients (in 12 of the 14 countries) started ESA treatment at registration and this increased to 31% at 24 months, combined with G-CSF in 7%. At registration, 29% of the patients had received at least one RBC transfusion with a mean pre-transfusion Hb level of 8 g/dL. The percentage of transfusion-dependent (TD) patients remained stable during follow-up with 31%, 29%, 26% and 29% at 6, 12, 18, 24 months of follow-up, respectively. At 24 months, overall survival (OS) is 83%. Median time from date of inclusion until progression to higher risk MDS or leukemia is 293 days. Most patients (123) have died without disease-progression (DP) versus 45 patients who have died after DP at 24 months (Table1). DP has been defined as an increase in bone marrow blasts to a higher WHO category. The main causes of death in patients without DP were infections (21%) and cardiovascular events (11%). The mortality rate in transfusion-independent (TI) and TD patients without DP was 5% and 24%, respectively. In TI and TD patients with DP, the mortality rate was 32% and 66%, respectively (Table1; Graph 1). To define the prognostic relevance of serum ferritin (SF) and TD, the SF levels divided in two groups (1. <1000 μg/L, 2. ≥1000 μg/L) were compared in TI and TD patients and stratified by disease-progression. The mortality rate according to SF at registration in TI patients without DP was 9% and 13%, respectively (HR 1.61, 95%CI 0.49–5.37). The mortality rate according to SF at registration in TD patients without DP was 21% and 56%, respectively (HR 4.79, 95%CI 2.56–8.96) (Table 1).
The great majority of deceased lower risk MDS patients have died before they have developed clinical signs of disease-progression. Transfusion-dependent patients without disease-progression have a four times higher mortality rate than transfusion-independent patients. This indicates that the pathophysiology of cytopenias and related complications are a major point of interest in early mortality, especially in patients without disease-progression.
Overall Survival at 2 years, stratified by disease-progression
| . | Total . | No Progression . | Progression . | ||
|---|---|---|---|---|---|
| . | Died . | Overall survival HR (95% CI)1 . | Died . | Overall survival HR (95% CI)1 . | |
| N | 1000 | 123 | 45 | ||
| IPSS score: | |||||
| 0 | 484 | 52 | 1 | 8 | 1 |
| 0.5 | 314 | 42 | 1.44 (0.96–2.16) | 17 | 0.55 (0.22–1.34) |
| 1 | 137 | 22 | 1.88 (1.14–3.09) | 14 | 1.52 (0.59–3.89) |
| WPSS score: | |||||
| Very Low | 316 | 29 | 1 | 4 | 1 |
| Low | 378 | 53 | 1.5 (0.95–2.38) | 17 | 0.48 (0.15–1.56) |
| Intermediate | 191 | 22 | 1.41 (0.81-2.46) | 13 | 1.1 (0.33-3.68) |
| High | 39 | 12 | 4.2 (2.14–8.26) | 5 | 1.84 (0.45–7.55) |
| Transfusions2: | |||||
| No | 540 | 28 | 1 | 7 | 1 |
| Yes | 460 | 95 | 4.12 (2.65–6.4) | 38 | 1.51 (0.64–3.56) |
| Transfusion-dependent: | |||||
| Ferritin at registration | |||||
| 1. <1000 μg/L | 176 | 33 | 1 | 13 | 1 |
| 2. ≥1000 μg/L | 43 | 18 | 4.79 (2.56–8.96) | 9 | 0.76 (0.26–2.21) |
| . | Total . | No Progression . | Progression . | ||
|---|---|---|---|---|---|
| . | Died . | Overall survival HR (95% CI)1 . | Died . | Overall survival HR (95% CI)1 . | |
| N | 1000 | 123 | 45 | ||
| IPSS score: | |||||
| 0 | 484 | 52 | 1 | 8 | 1 |
| 0.5 | 314 | 42 | 1.44 (0.96–2.16) | 17 | 0.55 (0.22–1.34) |
| 1 | 137 | 22 | 1.88 (1.14–3.09) | 14 | 1.52 (0.59–3.89) |
| WPSS score: | |||||
| Very Low | 316 | 29 | 1 | 4 | 1 |
| Low | 378 | 53 | 1.5 (0.95–2.38) | 17 | 0.48 (0.15–1.56) |
| Intermediate | 191 | 22 | 1.41 (0.81-2.46) | 13 | 1.1 (0.33-3.68) |
| High | 39 | 12 | 4.2 (2.14–8.26) | 5 | 1.84 (0.45–7.55) |
| Transfusions2: | |||||
| No | 540 | 28 | 1 | 7 | 1 |
| Yes | 460 | 95 | 4.12 (2.65–6.4) | 38 | 1.51 (0.64–3.56) |
| Transfusion-dependent: | |||||
| Ferritin at registration | |||||
| 1. <1000 μg/L | 176 | 33 | 1 | 13 | 1 |
| 2. ≥1000 μg/L | 43 | 18 | 4.79 (2.56–8.96) | 9 | 0.76 (0.26–2.21) |
Hazard Ratio (HR) (95% Confidence Intervals (CI)): IPSS, WPSS score adjusted for age, sex, country;
Transfusions, TD and Ferritin adjusted for age, sex, country, WHO category, cytogenetics, cytopenias, % blasts
At least one red blood cell transfusion recorded at registration or follow-up
Overall Survival stratified by disease-progression and RBC transfusions
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal