Abstract
Abstract 3800
Treatment of anemia in pts with myelodysplastic syndromes (MDS) may require packed red blood cell transfusion. Transfusion dependence in MDS is associated with poorer clinical outcomes and reduced overall survival (OS). This US registry prospectively collected data on clinical outcomes in chelated and non-chelated, transfused, lower-risk MDS pts. OS, leukemic transformation, and clinical events are reported for non-chelated and chelated pts at 36 mos on study.
This 5-year, non-interventional registry enrolled 600 pts from 107 US centers. Pts were ≥18 years old with lower-risk MDS (WHO, FAB, and/or IPSS) and transfusional iron overload (serum ferritin ≥1000 μg/L and/or ≥20 packed red blood cell units and/or ≥6 units every 12 weeks). The chelated group included all pts who had ever used iron chelation; sub-analysis was performed on pts with ≥6 mos chelation. Assessments were every 6 mos for 5 years or until death and included demographics, survival, disease status, comorbidities, causes of death, and MDS therapy.
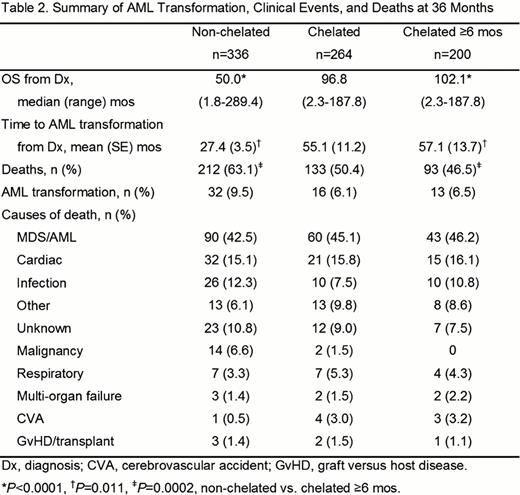
Baseline demographics and IPSS risk status were similar between groups, although transfusion burden trended higher in chelated pts (Table 1). As of April 30, 2012, 169 pts continued on registry, and 431 discontinued (345 died, 57.5%; 61 lost to follow-up, 10.2%; and 25 other, 4.2%). In all, 264 (44%) pts received chelation therapy; 200 had ≥6 mos chelation. OS and time to acute myeloid leukemia (AML) transformation were significantly longer, and percentage of deaths was significantly lower in chelated ≥6 mos vs. non-chelated pts (P<0.0001, P=0.011 [median not reached in either group], P=0.0002, respectively; Table 2). AML transformations were also lower in chelated ≥6 mos pts (not significant [NS]). Cardiac (non-chelated, 51.5%; ≥6 mos chelation, 30.5%) and vascular disorders (non-chelated, 59.2%; ≥6 mos chelation, 45.5%) were more prevalent in non-chelated pts at baseline; this trend continued on study: cardiac (non-chelated, 49.7%; ≥6 mos chelation, 42.5%); vascular (non-chelated, 55.7%; ≥6 mos chelation, 48.5%; NS, all comparisons). Most frequent causes of death were MDS/AML, cardiac events, and infection. The percentage of pts who had ever received MDS therapy was lower among non-chelated pts (non-chelated, 88.4%; ≥6 mos chelation, 93.5%; NS).
At 36 mos, chelated pts had significantly longer OS and time to AML transformation, as well as significantly fewer deaths. Trends toward fewer AML transformations and cardiac disorders were observed in chelated pts. Baseline characteristics and IPSS risk status were similar between groups, with the exception of more prevalent cardiac and vascular comorbidities in non-chelated pts. Additional assessments over the 5-year duration of this registry will provide further information on the association between chelation and clinical outcomes.
Summary of AML Transformation, Clinical Events, and Deaths at 36 Months
Lyons:Novartis: Research Funding; Amgen: Consultancy, Research Funding; Incyte: Consultancy, Research Funding; Telik: Research Funding. Paley:Novartis: Employment. Esposito:Novartis: Employment. Garcia-Manero:Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal