Abstract
Abstract 3775
In chronic myeloid leukemia (CML), achievement of optimal responses by time point has improved long-term outcomes. In contrast, several clinical studies investigating the clinical implications of suboptimal response showed that patients with suboptimal responses tend to have poor long-term outcomes. In IRIS study, patients who achieved major molecular response (MMR) at 18 months had event-free survival (EFS) benefit, compared to those who achieved complete cytogenetic response (CCyR) without MMR. However, the best treatment for these patients is still not confirmed. By the previous studies, sustaining standard-dose of imatinib (IM) is expected to yield less than 20 percent of additive MMR. In this prospective study, we investigated whether switching to nilotinib (NIL) or high-dose IM may be more effective for patients with suboptimal molecular response to IM as first-line therapy.
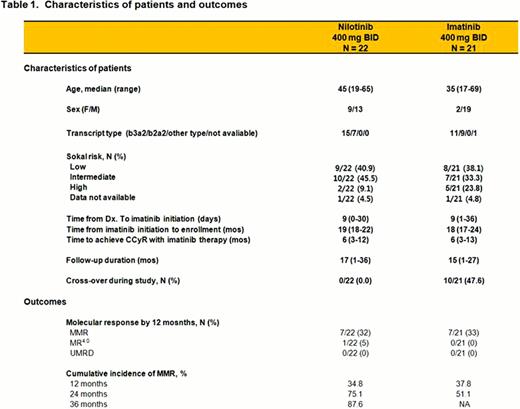
Early chronic phase (CP) CML patients who have achieved CCyR but no MMR after at least 18 months and up to 24 months (≤ 18 to ≥24 months) on first-line IM therapy at a daily dose of 400 mg were enrolled in this clinical trial, and informed consents were obtained from all patients. In NIL arm, patients received oral dose of 400 mg BID (800 mg/day) and in high-dose IM arm, patients received 800 mg/day administrated as 400 mg BID. Primary endpoint is to evaluate the cumulative MMR rates by 12 months, and secondary endpoints are to evaluate the cumulative MMR, MR4.0 and undetectable molecular residual disease (UMRD) rates during further 24 month follow-up. Safety profiles will also be assessed. Patients showing lack of response (lack of complete hematologic response (CHR) at 6 months, increasing WBC, no major cytogenetic response (MCyR) at 24 months), loss of response (loss of CHR or MCyR) or severe intolerance to treatment were allowed to crossover to the alternative treatment.
With a data cut-off date of 10 Jul 2012, a total of 43 patients were randomized into NIL arm (n = 22) or high-dose IM arm (n = 21). With a median follow-up of 15 months (range, 1–36), all patients have maintained CCyR without progression to advanced disease, and progressive decrease in BCR-ABL1 transcript levels was observed in all patients. Cumulative incidence (CI) of MMR by 12 months showed no significant difference between NIL arm and high-dose IM arm (37.8 ± 11.9% vs 34.8 ± 10.6%, P = 0.789). In NIL arm, 3 in 22 (14%) and 2 in 22 (9%) patients achieved MR4.0 and UMRD, respectively, and in high-dose IM arm, 1 in 21 (5%) patients achieved MR4.0. Overall, the patients treated with high-dose IM showed toxicities more frequently, such as fatigue, dyspnea and decreased phosphate. In addition, 10 patients in high-dose IM arm have cross-over to NIL treatment due to lack of response (n=9) and intolerance (n=1), and the median duration of NIL treatment was 14 months (range, 7–26 months). Among them, 5 (50%) patients have achieved MMR with a median NIL treatment duration of 12 months (range, 3–18).
These results demonstrate that early switching to NIL or dose escalation of IM could be recommended, considering the results of standard dose of IM in suboptimal molecular responders. When the tolerability of treatment was considered for switching to NIL or high-dose IM, NIL may be preferred. Through further clinical investigation on a large patient population and longer period observation, the efficacy and safety of early intervention of suboptimal molecular response using NIL or dose escalation of IM will be needed. Updated data with longer follow-up duration will be presented in the meeting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal