Abstract
Abstract  3756
3756
The introduction of second generation tyrosine kinase inhibitors (TKI2) in the treatment of chronic phase chronic myelogenous leukemia (CML) has improved the response rates in the second, and now, in the first line setting. Nilotinib, a TKI2 with a restricted kinase inhibition profile, demonstrated higher rates of response over imatinib (IM) as front line therapy with a very good short-term tolerability profile. Even if the proportion of patients (pts) in undetectable disease increases with time, the majority will have to continue this treatment for several yrs to avoid progression. In this perspective, mid- and long-term safety issues are of concern, and recent reports point out the onset of arteriopathies in such pts with a suspected abnormal frequency.
We have prospectively analysed our on-nilotinib cohort of CP CML between September 2011 and July 2012 with standard clinical assessments [height, weight, body mass index (BMI), ankle-brachial index (ABI)], and basic routine metabolic laboratory assessments (fasting glucose, total, HDL and LDL cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, glycosylated hemoglobin) and BCR-ABL (IS), to explore and detect at early stages abnormalities that may have some later cardio-vascular consequences for pts on this drug.
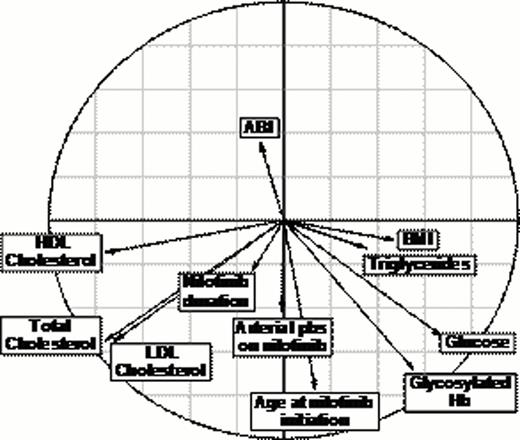
We analysed a series of 54 CML pts all in CP. The median age at diagnosis was 50 (18–73) and 55 (20–78) yrs at nilotinib initiation. The Sokal score was low for 27%, intermediate for 55%, high for 8%, unknown for 10 pts. At CML diagnosis, 13 pts had hypertension, 4 diabetes mellitus, 2 previous peripheral arterial disease (PAD), 4 coronary artery disease (CAD), and 9 pts had tobacco addiction. Thirty-seven pts had IM first line for a median of 4.2 (0.2–11) yrs, then nilotinib for IM-intolerance (14 pts) or IM-resistance (16 pts), or entering a clinical trial (5 pts) and 2 for unknown reasons for a median of 2.8 (0.5–5.6) yrs. Seventeen pts had nilotinib first line for a median of 1 (0.3–4.7) year. The disease duration ranged from 0.4 to 19.3 yrs (median 5.6). Overall, the median duration of nilotinib was 2.2 (0.3–6.8) yrs. Two pts were in CHR, 11 pts in CCyR, 28 in MMR, 13 in undetectable disease (MR4.5) at assessment. In pts on nilotinib without statins at time of assessment, 62% (n=40) showed high total cholesterol values (>2 g/l), 46% (n=37) had high LDL cholesterol (>1.5 g/l) and 57% (n=37) low HDL cholesterol values (<0.6 g/l). Triglycerides were high (>1.48 g/l) in 18% of pts (n=49). Glycosylated hemoglobin was high (>6%) in 18% of the pts treated (n=38), and glucose (> 5.8 mmol/l) in 20% (n=11). Seven pts (13%) were overweight (BMI>30) and the median BMI was 24.6 (16.7–47). On 54 pts, 25% of pts (n=13) had an abnormal ABI (<1) and true arterial problems were authentified by Doppler ultrasound in 13% (n=7) of pts after a median of 2.6 (0.6–4.4) yrs of nilotinib: carotid atherosclerosis, inflammatory carotiditis, one CAD, 4 PADs, with 5 newly diagnosed on nilotinib. In order to correlate the different parameters together we use the correlation circle strategy (see figure 1 below) resulting from the principle components analysis (PCA), in this circle each arrow represents a studied parameter, and the closest one parameter is to another one, the closest the arrows are. Perpendicular arrows denote no correlation at all. The length of each arrow depends on the weight of each parameter compared to the others within the PCA.
Correlation circle for the different parameters studied (“Hb” states for Hemoglobin, “pbs” for problems, “ABI” for ankle-brachial index, “BMI” for body mass index).
Correlation circle for the different parameters studied (“Hb” states for Hemoglobin, “pbs” for problems, “ABI” for ankle-brachial index, “BMI” for body mass index).
As seen; there is a strong correlation between the duration of nilotinib and the total cholesterol, high LDL cholesterol, arterial problems and age at nilotinib initiation. ABI failed in detecting authentified arterial problems detected by other means. The Pearson correlation test nearly reached statistical significance between nilotinib duration and arterial problems (p=0.07).
In conclusion, nilotinib induces clear metabolic disturbances along treatment, particularly for lipids and glucose parameters, which can be responsible for significant arteriopathies, that ABI failed to detect. These results should promote the lipids and glucose parameters follow-up during CML treatment by nilotinib in order to detect disturbances at early times, correct them using strict dietary rules and/or concomitant medications to avoid arterial problems at later time points.
Nicolini:Novartis, Bristol Myers-Squibb, Pfizer, ARIAD, and Teva: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal