Abstract
Abstract 3703
Local intratumoral injection of CpG ologonucleotides in conjunction with local low dose radiotherapy can induce regression of uninjected distant sites of disease in patients with follicular lymphoma (FL) (Brody et. al JCO). This maneuver activates the Toll-like receptor 9 (TLR9) within the tumor cells and in adjacent antigen presenting cells in the local tumor environment, such as dendritic cells and macrophages. A systemic anti-tumor T cell immune response is thereby induced. Our original phase I/II trial was conducted in patients who had been previously treated with standard therapies and had recurred with multiple sites of disease. We observed significant clinical responses as well as anti-tumor T cell immune responses as measured in vitro using peripheral blood T cells or T cells obtained from a pleural effusion adjacent to a responding tumor site.
We now extended the trial of in situ vaccination to newly diagnosed patients prior to any other therapy, a group that may have a more intact immune system. Patients were eligible if they had FL grades I-IIIa, stage III or IV and were not in need of immediate treatment. One involved lymph node was biopsied and viable suspensions of tumor cells were prepared and cryopreserved for use as stimulators in immune assays. A second site received low dose XRT (2Gy on each of two successive days) together with 10 weekly injections of 18mg of CpG ologonucleotide (PF-3512676, Pfizer) all into the same tumor site, beginning on the second day of XRT. Peripheral blood lymphocytes (PBL) were obtained prior to each injection and two weeks after the last injection. These were cryopreserved and used as responder cells for assays of T cell immune responses.
We sought to determine the kinetics of anti-tumor T cell immune responses as well as which type of T cell response that was the most informative.
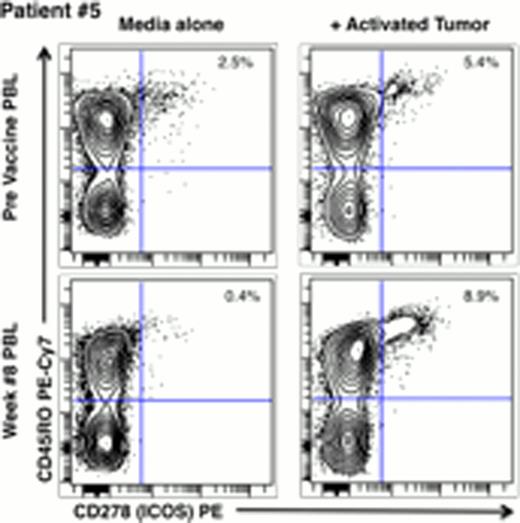
Tumor cells were thawed and activated for 3 days with CpG and soluble CD40L. They were then incubated for 5 days with autologous PBL T cells. Fresh stimulator cells were then added for a final overnight culture. Responding T cells were stained for subtype (CD4, CD8, CD56, CD45RO), for their expression of activation markers (CD25, CD137 and CD278), for their expression of intracellular cytokines (IFN-g, TNF and IL-2), and for their expression of cytotoxic enzymes (perforin and granzyme B). The cells were then analyzed by multiparamer flow cytometry (BD LSRII). For measurement of perforin and granzymeB, the cells were gated on CD8+/CD3+/CD56- to exclude NK cells.
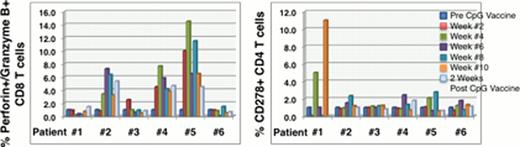
In response to in situ vaccination, all patients made anti-tumor immune responses. Some generated only CD4 responses, some only CD8 responses and others made both CD4 and CD8 T cell responses. Representative data are shown in the figures below. We found that for CD4 responses the activation marker CD278 (ICOS) was particularly informative, and usually restricted to the CD45RO+ memory subset. For CD8 responses, the most robust readout was intracellular expression of the combination of Perforin and Granzyme B.
CD8 Immune responses became positive as early as two weeks after the start of vaccination. CD4 responses became positive by four weeks of vaccination.
As in our previous trial, we observed clinical responses, with regression of tumors at uninjected/untreated sites of disease. An evaluation of the magnitude and duration of these clinical responses and their relation to immune parameters awaits a more extended time of followup.
In situ vaccination efficiently induced immune responses in previously untreated patients with FL. These responses occurred within two weeks after initiation of vaccination. The immune responses was heterogeneous and included both CD4 and CD8 T cells. The most robust measures of T cell response will be correlated with clinical outcome. The identification of a limited panel of correlative immune response markers and an understanding of the response kinetics will allow a focused approach to immuno-monitoring in future clinical trials.
Advani:Pharmacyclics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal