Abstract
Abstract 3675
Mantle cell lymphoma (MCL) remains incurable and little consensus exists on the best standard initial therapy. However, improved understanding of disease biology has the potential to lead to novel treatment approaches including new perspectives on older drugs. For example, epigenetic modifications including altered DNA methylation and histone acetylation previously identified in MCL has provided the rationale for using the combination of a hypomethylating agent and a histone deactylase inhibitor. Here we show that agents with differing mechanisms have significant activity in previously untreated MCL.
In addition to its cytotoxic effects in lymphoid malignancies, cladribine has hypomethylating properties. Vorinostat (SAHA) is a histone deacetylase inhibitor (HDACi) FDA approved in cutaneous T cell lymphoma with modest single agent activity in MCL. Preclinically, the combination of these agents has been shown to activate silenced genes. Since cladribine inhibits DNA methylation via a unique mechanism, it could also potentially inhibit histone methylation.
We previously reported initial results of our Phase I/II trial combining SAHA, cladribine, and rituximab (SCR) for the treatment of B-cell non-Hodgkin's Lymphoma (NHL) [Spurgeon et al, ASH, 2012]. Here we present the updated results from the Phase II portion of the trial in the untreated MCL cohort including response rate, overall and progression free survival, and correlative studies.
The achieved phase II starting dose was vorinostat 400 mg po (days 1–14) combined with cladribine 5mg/m2 IV (days 1–5), and Rituximab 375 mg/m2 IV (weekly × 4 for cycle 1 and 1x/month) every 28 days for up to 6 cycles. Response evaluation occurs after 2 cycles and at the completion of therapy. Responding patients are eligible to receive maintenance rituximab. Phase II eligibility includes relapsed NHL as well as previously untreated MCL. The primary outcome is response rate (ORR); secondary endpoints include progression-free survival (PFS) and overall survival (OS). Scientific correlatives include analysis of CD20 expression, histone acetylation, gene microarray, qRT-PCR and HELP methylation analysis. To evaluate the possible effects of SAHA metabolism on toxicity and response, UDP-glucuronosyltransferase 2B17 (UGT2B17) genotyping is also performed. This study continues to enroll patients.
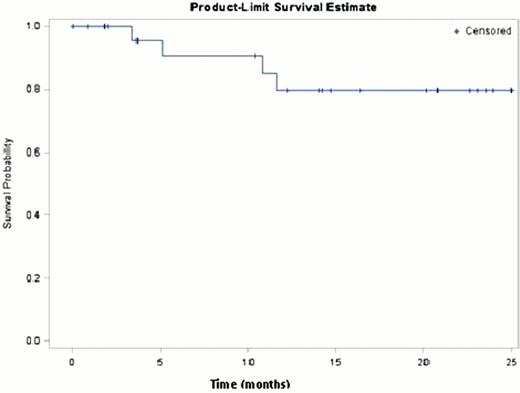
28 previously untreated MCL patients have been enrolled on the phase II portion of the study. 7 have not yet completed the planned 6 cycles; however, 26 patients have completed ≥ 2 cycles and are evaluable for response. The majority of responding patients have received maintenance rituximab. The overall response rate (ORR) is 100% (26/26) with 69% (18/26) achieving CR. Of those patients not attaining CR, 2 had blastic MCL and died, 3 have not yet completed active treatment, and 1 withdrew consent after two cycles. At a median follow up of 14.7 months (.07 – 25 months) 4 patients have relapsed and 3 have died. Of the relapsing patients, two had blastic MCL. None of the patients achieving a CR has relapsed. The estimated PFS curve (shown in the Kaplan-Meier curve below) did not reach the 0.5 level and therefore, median PFS could not be estimated. Toxicities were defined using CTCAE 4 and primarily include neutropenia, thrombocytopenia, fatigue, anorexia, and dehydration.
We found that cladribine hypomethylates DNA in vivo (8/8 pts) and inhibits histone methylation in vitro. There were no upregulated genes common to untreated leukemic MCL patients; however, a number of changes in gene expression were observed. For example, upregulated genes after treatment included DUSP2 (3 patients), FOXO3 (2 patients), NOXA1 (2 patients), CEBPb (2 patients) and p53 (3 patients).
The SCR regimen has significant activity and shows epigenetic activity in previously untreated MCL. Initial follow up results are promising, especially in patients without blastic MCL who continue with maintenance rituximab. The SCR regimen should be studied further in NHL.
Spurgeon:Merck : Research Funding. Off Label Use: vorinostat: off label use mantle cell lymphoma. Epner:Merck: Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal