Abstract
Abstract 3653
The rearrangement Bcl2/IgH is detectable by PCR in more than half of patients with follicular lymphoma. Different authors reported on the long-term prognostic impact of the persistence of this rearrangement (minimal residual disease or MRD). In this study, we report about MRD significance in 534 patients randomized to receive 8 doses of Rituximab associated with 8 cycles of CVP, or 6 cycles of CHOP or FM, and no maintenance in the context of the Fondazione Italiana Linfomi (FIL) multicenter phase-III “FOLL05” trial (NCT00774826).
For qualitative PCR analysis, samples were centralized.
Quantitative assays were performed by the 4 laboratories of the “FIL MRD NETWORK”. Qualitative and quantitative PCR were performed according to the Euro-MRD guidelines.
At baseline, 424 out of the 504 patients enrolled were assessed for Bcl2/IgH and 223 (52,6%) were Bcl2/IgH positive (molecular marker=MM). No significant differences were detected between cases with and without molecular assessment at the enrollment or after therapy, and those with positive or negative MM for the main clinical and prognostic features, and for treatment allocation.
At the first time-point (within 6 weeks after the end of therapy), 153 of the 223 cases PCR-positive at enrollment were re-assessed: 110 (69,6%) achieved PCR negativity. MRD was not significantly correlated to clinical features or quality of clinical response.
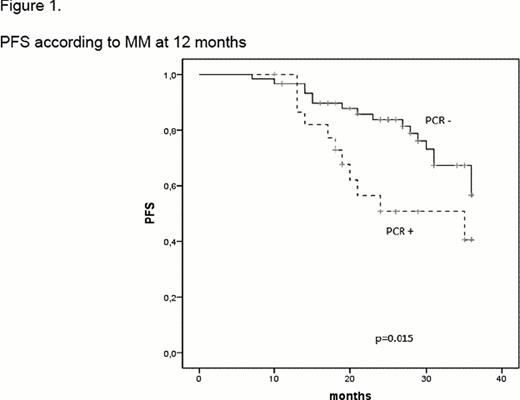
Three-year PFS was better for patients achieving PCR negativity at the sixth week than those retained MM (69% vs 50%), but this difference was not statistically significant. On the contrary, PFS was significantly conditioned by the PCR status at 12 and 24 months (87 and 66 cases evaluable), with 3-year PFS of 66% for cases PCR-negative versus 41% for those PCR-positive at 12 months (p=0.015, see Figure 1), and 84% vs 50% (p=0.014) at 24 months.
Moreover, the probability of being PCR-negative by 24 months was significantly lower for cases receiving R-CVP (18% vs 41% in the R-CHOP and 41% in the R-FM, p=0.035).
PCR-negativity resulted in better PFS both in CR and in PR patients (3-year PSF=72% for cases CR/PCR- vs 32% for those CR/PCR+ vs 62% for those PR/PCR- and 25% for patients in PR/PCR+; p=0.001).
When PCR negativity in patients with or without complete response and PCR negativity by 12 months were considered in a multivariate analysis together with performance status, FLIPI, response, and age, the PCR negativity retained its favorable impact on PFS (HR=-1.2, 95% CI:0.32–0.19, p=0.001).
Finally, in 105 cases tumor burden at the diagnosis was assessed by quantitative PCR. The median value was 3 × 10−3 copies; cases displaying values <1 × 10−4 showed a clear advantage in terms of PFS (3-year PFS of 80% vs 59% for those with >1 × 10−4 copies p=0.015).
A significant MRD clearance was observed at the end of therapy: the mean value of Bcl2/IgH was 2 × 10−1 copies before therapy versus 5 × 10−3 at the first time-point. No differences in the entity of the MRD clearance were observed according to the arm of treatment.
In conclusion, this study shows that R-CHOP and R-FM are more effective to clear MRD in follicular lymphoma compared to R-CVP.
Moreover, the most prominent impact on PFS is exerted by the molecular status detected at least 6 months after the end of therapy. This observation is in line with the hypothesis of a quite slow, but long-term sustained, MRD clearance exerted by rituximab-based therapies.
Finally, this study shows that patients with <1 × 10−4 copies of Bcl2/IgH at diagnosis would have longer PFS, thus supporting the usefulness of a quantitative PCR monitoring at diagnosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal