Abstract
Abstract 361
Patients with deep vein thrombus (DVT) can safely be treated as outpatients using subcutaneous low molecular weight heparin (LMWH). However the role of outpatient treatment in patients diagnosed with a pulmonary embolism (PE) is controversial. This practice is not accepted in many centers and majority of patients are still admitted to the hospital for observation. Clinicians are reluctant to discharge patients due to insufficient data supporting the safety of outpatient management of PE.
To determine the safety of outpatient treatment of acute symptomatic PE and the outcomes associated with outpatient management of PE including venous thromboembolism (VTE) recurrence, major bleeding, fatal PE, fatal intracranial hemorrhage (ICH), and overall mortality.
A systematic literature search strategy was conducted using MEDLINE, EMBASE, the Cochrane Register of Controlled Trials and all EBM Reviews of published studies up to June 2012. We included randomized controlled trials (RCTs) and prospective cohort studies. We calculated the pooled proportions for the different outcomes at 3-months of follow-up. Ninety-five percent confidence intervals (95% CI) were calculated for each rate using the averaged, inverse variance-weighted estimates from each study.
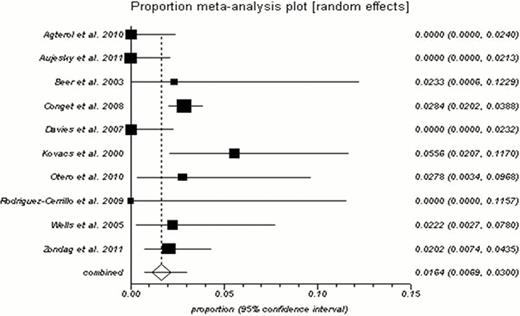
Thirteen studies met all the inclusion criteria (3 RCTs and 10 prospective cohort studies). A total of 2458 patients were included in the systematic review. Different risk stratification methods were used to identify low risk patients with PE such as the pulmonary embolism severity index (PESI), the Geneva prognostic score, clinical gestalt and/or laboratory markers. The risk of recurrent VTE in patients with PE managed as outpatients was 1.64% (95% CI 0.69 – 3.0%; I2: 70.7%) during the 3 months follow-up period. The rate of fatal PE was 0.70% (95% CI 0.14 – 1. 7%; I2: 72.6%). The rates of major bleeding and ICH were 1.14% (95% CI 0.35 – 2.34%; I2: 72.8%) and 0.29% (95% CI 0.06– 0.68%; I2: 0%), respectively. The overall mortality rate was 2.3% (95% CI 0.41 – 5.7%; I-square: 92.8%). The I2 was moderate to high for most proportions, likely due to difference in the baseline characteristics (e.g. the inclusion of cancer patients in some studies).
Independent of the risk stratification methods used, the rate of adverse events associated with outpatient PE treatment seems low. Based on our systematic review and pooled meta-analysis, numerous patients with acute PE can safely be treated as outpatients.
Proportion meta-analysis showing the risk of recurrent VTE in patients with PE managed as outpatients for a 3 month follow up period.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal