Abstract
Abstract  3553
3553
The absolute lymphocyte count (ALC) has been shown to be a predictor of event free survival in the post transplant setting in many diseases including lymphoma, myeloma and leukaemia. (Porrata et al). Studies carried out at Alder Hey Childrens' Hospital, Liverpool in 2003 was the first one of its kind in looking at the ALC as a prognostic tool in the non-bone marrow transplantation setting in childhood leukaemia (Lomas et al, Hudson et al). The studies in acute myeloid leukaemia were small with short follow up. We present here the largest study of the prognostic significance of ALC in paediatric Acute Myeloid Leukaemia.
We perfomed a retrospective single centre study involving 59 paediatric patients diagnosed with Acute Myeloid Leukaemia between 1985 and 2010 and treated using Medical Research Council AML 10, AML 12 and AML 15 protocols. Data was analysed for event free and overall survival. All 28 deaths occurred within 3 years. Follow up was 11 months to 27 years in the 31 survivors.
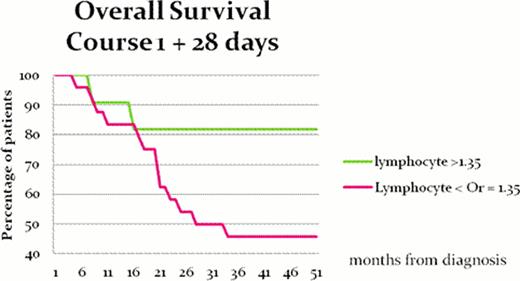
A clear relationship was observed between patients with higher absolute lymphocyte counts and overall and event-free survival At 28 days post course 1 chemotherapy, using an ALC threshold value of 1.35 × 109/L, overall survival is 82% v 47% (p = 0.0336). The effect of the ALC diminishes with subsequent chemotherapy courses. At 28 days post course 2 chemotherapy using an ALC threshold value of 1.22 × 109/L, overall survival is 65% v 36% (p = 0.2952). At 28 days post course 4 chemotherapy using an ALC threshold of 0.67 × 109/L, overall survival is 69% v 50% p = 0.5983.
We hypothesise that the higher ALC in the event-free patients, is due to tumour specific lymphocyte proliferation, causing clearance of low levels of leukaemia after chemotherapy. The chemotherapy acts to cause leukaemia cell death and antigen processing through macrophages. Chemotherapy causes tissue damage leading to upregulation of immunological danger signals with T and B lymphocyte expansion with specificity against the residual leukaemia cells. The reduced effect of the ALC predicting survival with each subsequent course of therapy may be a result of less leukaemia cells being present prior to each course. Less leukaemia cell death with each course results in less leukaemia antigen processing, presentation and lymphocyte expansion. If this hypothesis is confirmed it may be possible to carry out harvesting of tumour specific lymphocytes prior to chemotherapy with post chemotherapy add back to enhance the curative effect.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal