Abstract
Abstract 3123
Multiple myeloma (MM) is a plasma cell malignancy with variable prognosis depending on disease features such as β2m level and cytogenetics. High dose therapy and stem cell transplantation (SCT) remains the current standard of care for MM, however the role of tandem SCT is controversial, particularly in the era of novel induction therapy.
The Virginia Commonwealth University BMT program has a practice of risk-stratified transplant allocation in MM patients referred for SCT; those with high-risk (HR) disease (β2m >5.5, adverse cytogenetics, >1st remission) are preferentially assigned tandem SCT, and those with standard-risk (SR), a single SCT. Between 2008 and 2011, 146 MM patients underwent SCT, 64 (44%) SR patients received a single SCT (SRS), 32 (22%) HR patients received tandem SCT (HRT) & 50 (34%) a single SCT (HRS). Median age at SCT was 58 years. Maintenance therapy was administered in 48% SRS, 53% HRT & 63% HRS patients.
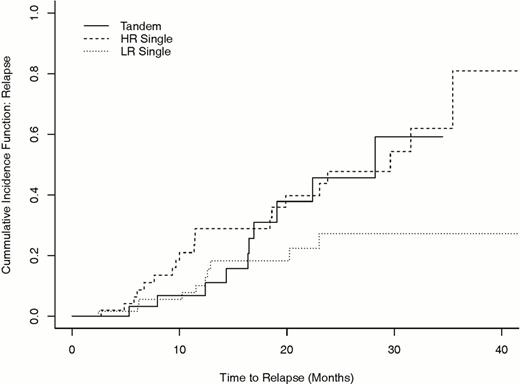
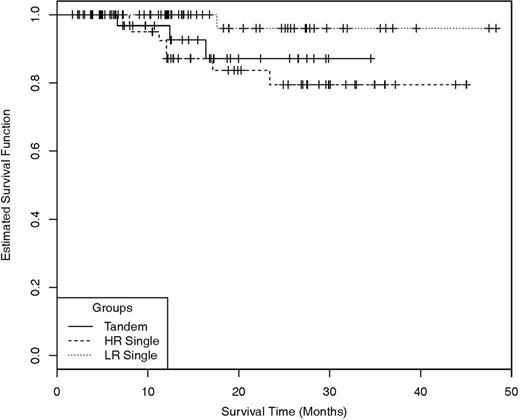
Disease status at day 100 post-transplant was complete response (CR) or very good partial response (VGPR) in 84%, 75% and 72% patients in the SRS, HRT, and HRS groups respectively. Patients in the HRT group (41%) were more likely to achieve CR than in the HRS group (18%) (P=0.04). At a median follow up of 23 months, there was no difference in the relapse incidence (Figure 1) between the HRT and SRS groups (Log Rank P=0.22) or between the HRT and HRS groups (Log Rank P=0.64), however the relapse incidence for SRS was lower than for HRS group (Log Rank P=0.01). Correspondingly, there is no difference in the estimated survival between the HRT and SRS (Log Rank P=0.12), or between the HRT and HRS groups (Log Rank P=0.57), though the survival for the SRS group is superior to HRS group (Log Rank P=0.025) (Figure 2). Estimated 2-year survival rates are 0.96 (95% CI: 0.88, 1.00), 0.87 (0.73, 1.0), and 0.79 (0.65, 0.94) in the SRS, HRT and HRS groups respectively, where the SRS survival is significantly higher than the HRS group (Log Rank P=0.047). This was attributable to a lower 1-year relapse rate of 0.10 (0.02, 0.19), 0.07 (0.00, 0.16) in the SRS, HRT groups compared to 0.29 (0.15, 0.43) in the HRS group (Log Rank P<0.03). Further analysis accounting for group status revealed that HR patients with IgA subtype, <CR/VGPR status, absence of bortezomib pre-SCT and absence of maintenance therapy post-SCT all experienced a higher rate of relapse (P <0.05, Cochran- Mantel-Haenszel test). Similarly, patients with <VGPR, and absence of maintenance therapy had an inferior survival.
We report that HR MM patients undergoing tandem transplant have a higher response rate and thus a correspondingly lower relapse risk and improved survival comparable to SR. Therefore risk stratification in patients with MM using simple clinical and laboratory parameters may be used to guide single versus tandem SCT allocation. HR MM patients who cannot get tandem transplant for insurance or clinical reasons may benefit from receiving bortezomib as part of pre-transplant therapy with a goal to achieve maximal cytoreduction. Further benefit in these patients may be derived from post-transplant maintenance therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal