Abstract
Abstract 3102
Identifying the optimal patients and timing for allogeneic hematopoietic stem cell transplant (HSCT) is an ongoing challenge for transplant centers that requires assessment of more than just the disease status and stage. Pre-existing co-morbidities also independently impact both 100 day and 1 year non-relapse mortality (NRM) as well as long term overall survival. Additionally, the CIBMTR has also shown that Hispanic patients have an inferior survival after allogeneic HSCT, although why ethnicity is linked to a higher mortality, e.g. is it higher risk/timing of transplant, lower socioeconomic status, increased co-morbidities, etc. however, is still undetermined. A survival analysis of allogeneic HCT outcomes that includes ethnicity, co-morbidity, insurance payor, as well as traditional risk factors such as age, disease risk at transplant, and remission status would be helpful to clarify the outcome disparities found in different ethnic subgroups and more importantly lead to strategies to minimize the effect.
We performed a retrospective analysis of the outcome of 363 consecutive adult allogeneic transplants at Loyola University Hospital of whom approximately 10% were Hispanics (34) from January 1, 2003 to June 30, 2010. We use a focused approach to optimize care of non-English speaking Hispanics which involves native speakers at all levels, written materials in Spanish, and an IRB approved method to permit all non-English speaking patients to enroll in all clinical trials is present. Traditional prognostic data as well as the Sorror co-morbidity index and socioeconomic and ethnicity status were determined for each patient. The surrogate we used for socioeconomic status was insurance payor (i.e. indigent + Medicaid vs. third party insurance/Medicare). Survival analysis was calculated using Kaplan Meier plots considering each patient at 100 days, 1 year, and 3 years.
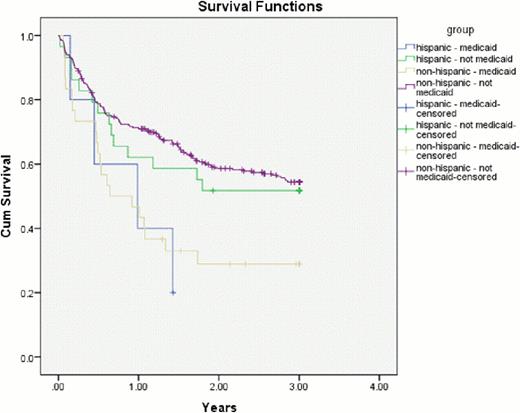
The median age for the 363 patients was 47.1 years with 48.7% being in the High Risk CIBMTR category, and 74.1% being in remission at transplant. The median co-morbidity index was 2.0. No differences were seen in remission status or the co-morbidity index for Hispanic vs. non-Hispanic patients, while fewer Hispanic patients were in the High CIBMTR Risk group (27.3 vs. 50.9%; p = .048). Survival for Hispanics (34) vs. non-Hispanics (329) showed no difference in overall survival at three years (42.1 vs. 42.8%). Based on payors, we found no statistical difference in 100 day overall mortality after HSCT for those with Medicaid (n = 35) vs. non-Medicaid (n = 328) payors with Hispanic non-Medicaid and non-Hispanic non-Medicaid survivals at 100 days of 82.8 and 87.9%. However despite the relatively small number, both the non-Hispanic and Hispanic patients with Medicaid showed a significantly decreased survival after 100 days with 3 year survivals of 20.0 and 30.0% for Hispanic and non-Hispanic Medicaid patients vs. 51.7 and 56.7% of the Hispanic and non-Hispanic non-Medicaid groups respectively (p = .002).
Unlike prior reports, and perhaps by using a focused approach for our non-English speaking Hispanic patients, we found no difference in survival between Hispanics and non-Hispanics in our series of 363 consecutive allografts at 100 days, 1, or 3 years, although they may have been predicted to have had a slightly better prognosis based on a better Risk Group status. We did however find that payor was an important prognostic variable for outcome after the first 100 days regardless of ethnicity. Whether this is simply due to the financial toll of such a chronic illness and therapy remains to be seen, but this suggests that closer follow-up after day 100 may be of significant benefit for this subgroup of patents which may grow due to health care reform.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal