Abstract
Abstract 305
Non-Hodgkin's lymphoma (NHL) are malignant tumors usually sensitive to chemotherapy; this results in prolonged survival and possibly disease eradication in a large proportion of patients. However, despite the general improvement in treatment options, a variable number of patients still shows a refractory disease, i.e. poor or absent response to induction therapy. Prediction and management of refractory disease is a major issue in the biological and clinical research programs for NHL. The present study was undertaken to evaluate on a large series of NHL patients, managed at two Italian centers over the last three decades: i. the actual rate of refractory patients; ii. the main factors associated with refractory disease; iii. the long-term outcome of refractory vs. responsive patients.
Data have been collected on a series of 3,952 NHL patients, referred and treated at the University Hematology of Torino (S. Giovanni B. and Mauriziano Hospitals) (864 cases) and at the Hematology Division of Ospedali Riuniti di Bergamo (3,088 cases), between 1984 and 2012. There were 1,819 (46%) female patients, 2,056 (52%) were aged less than 60 yrs, B-cell NHL were 3,633 (92%), with 318 (8%) patients diagnosed as T-NHL; main histological subtypes included: 1,809 (45.8%) Diffuse Large Cell Lymphoma (DLCL), 758 (19.2%) follicular lymphoma (FL), 210 (5.3%) mantle-cell lymphoma, the remaining 1,175 (29.7) had other histologies. According to Ann Arbor staging, 2,369 (62%) patients presented with advanced stage disease and 914 out of 2,174 evaluable patients (42%) had an intermediate-high IPI score. Overall, 1,430 out of 3,187 (44.9%) received conventional chemo-radiotherapy supplemented with rituximab. The criteria to identify refractory patients were: stable or progressive disease (fully refractory) or transient response with disease progression within 6 months (early relapse), following first-line chemotherapy.
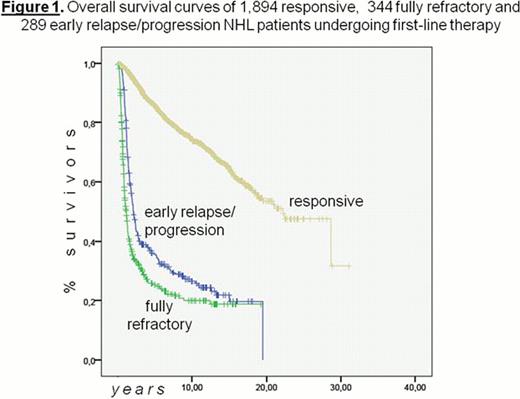
Among 2,543 broadly analysed patients, treated during the last 28 yrs, 649 (25.5%) were classified as refractory, including 14% fully refractory and 11.5% with early relapse or disease progression. The overall incidence of refractory disease was similar in the two Centers, 24.1% in Torino and 26.3% in Bergamo. The rate of refractoriness was as high as 46.9% in the small T-cell subgroup, while the overall incidence was 23.6% for B-cell NHL (p<0.001), with refractory patients more frequently observed among DLCL (26.0%) than in FL (15.1%) (p<0.001). Besides T-cell histology, the following factors had the highest association (p<0.001) with treatment response: i. intermediate-high risk IPI presentation, with 38.5% refractory patients, compared to 16.7% for 0–2 IPI scores; ii. female gender, with a markedly lower incidence (22%) of refractoriness compared to males (28.4%); iii. rituximab addition, that cut the incidence of refractoriness to 19.2% compared to 28.8% for patients treated without rituximab. These factors maintained their independent predictive values in multivariate regression analysis. At a median follow-up of 5.4 yrs., 1,607 (61%) out of 2,543 patients are alive, 11.8% of them were refractory to their first line treatment. Indeed, among 649 refractory patients, 189 (29%) are presently alive, compared to 1,418 alive (75%) among 1,894 responsive patients. Lastly, the overall survival (OS) was significantly poorer for fully refractory (median survival: 1.1 yrs) compared to early relapse patients (2.09 yrs) (p<0.001); both these refractory subgroups had a definitely poorer OS compared to responsive patients, whose median survival was 22.2 yrs (see Figure 1).
i. Overall, in this large series of NHL patients who received induction therapy both in the pre- and post-Rituximab era, approximately one fourth displays full refractoriness or early relapse/progression; ii. the introduction of rituximab has markedly reduced the risk of refractory disease, whose incidence is now around 19%; iii. a markedly higher rate of refractory disease is observed with T-subtypes compared to B-cell NHL; iv. intermediate-high IPI score is associated to refractoriness, while female gender significantly reduces the risk of refractory disease; iv. patients responsive to first-line therapy have a very prolonged life expectancy, with a median survival around 22 yrs, whereas the median survival for refractory patients does not exceed 2 yrs.
Tarella:Hoffmann-La Roche: Consultancy, Honoraria. Rambaldi:Hoffmann-La Roche: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal