Abstract
Abstract 3024
High dose melphalan supported by autologous hematopoietic cell transplantation has been shown to prolong survival and decrease relapse rates compared to conventional chemotherapies in elligible patients with multiple myeloma (MM) but unfortunately relapses remain a problem. Various factors have been shown to affect the relapse after transplantation. Malignant plasma cells (PCs) have been documented to contaminate blood stem cell harvest products. Conflicting results have been reported regarding the levels of PC contamination in apheresis products from patients with MM undergoing transplantation (Tx) and their impact on relapse and survival. Aim of this study was to analyze post induction residual myeloma by flow cytometric detection of the graft and by whole body PET imaging.
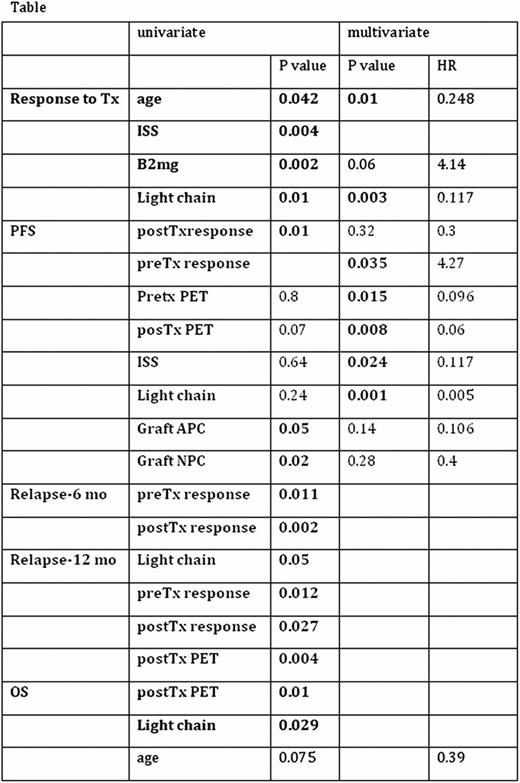
Standard panel was set up with CD138FITC/CD38PE/CD45ECD/CD56PC5. CD45negCD56pos plasma cells were identified as abnormal plasma cells. If any aberrant expression [such as CD20(loss) CD27(loss) CD28 (gain), CD33(loss), CD34 (gain), CD81(loss), CD117(gain)] is detected at diagnosis, the corresponding antibody was also added to the panel. Univariate and multivariate analysis were performed by SPSS.16.
Apheresis products from 118 patients (female/male=53/65; median age at diagnosis= 55 (35–69)) were tested for the presence of abnormal PCs and the number of normal PCs. The number of patients in MM subtypes IgG/IgA/Light chain/non-secretory were 70/20/26/2. International scoring system I/II/III:50/38/30. Most patients (n=108) had received one or two lines of induction and 52 had bortezomib based therapies before transplantation. In univariate analysis age (> 55; ≤ 55), ISS (ISS1 vs ISS2 + ISS3), beta2 mcg (>3.5 and ≤ 3.5) and MM Subtype (light chain vs others) were significantly associated with response to Tx. Presence of abnormal PCs in the harvests did not significantly affect response to Tx or OS. However, both the presence of abnormal PCs and the amount of normal PCs > 7.6 ×105/kg was associated with shorter PFS. Fifty-five of the patients had pre and post-Tx PET-imaging done. On the other hand, post-Tx PET positivity negatively affected the PFS. Post-Tx PET positivity was also significantly associated with relapse at 12 months after transplantation. Pre and post-Tx disease status significantly influenced relapse after transplantation. In multivariate analysis, age, beta2 mcg and light chain myeloma continued to be significantly associated with response to transplantation. Abnormal PC contamination and the amount of normal PCs> 7.6 ×105/kg were not associated with pre-Tx PET positivity.
Age, ISS, beta2 mcg, light chain disease are predictors of response to transplant. Response to the treatments before mobilization, response to Tx, post Tx PET positivity, graft plasma cell (abnormal or normal) content, serum LDH are predictors of PFS. Response (≥VGPR) during mobilization correlates with less abnormal plasma cells in the apheresis product. PC contamination of the graft does not prevent response to transplant. However, presence of abnormal PC in the apheresis product as well as PET positivity predicts shorter DFS compared to lack of residual disease by flow or PET imaging (11 vs 18 months).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal