Abstract
Abstract 2692
Massive splenomegaly is occasionally encountered in patients with Non-Hodgkin's Lymphoma (NHL) and can be associated with abdominal symptoms, anemia and thrombocytopenia. The spleen may also be a primary focus of the disease itself. Splenectomy offers the benefit of localized treatment of the disease as well as relief of symptoms from splenomegaly and associated cytopenias. The safety and long term clinical outcomes of splenectomy for massive splenomegaly (>1500 gm) in patients with various histologies of NHL was analyzed.
Data was obtained from clinical records of 90 patients with a diagnosis of NHL who underwent a splenectomy at Mayo Clinic Rochester from January 1998 to December 2007. Demographics, previous treatments, histology, post- surgical complications were collected and analyzed for the entire cohort. Additionally, median overall survival, improvement in symptoms, anemia and thrombocytopenia were analyzed by NHL type.
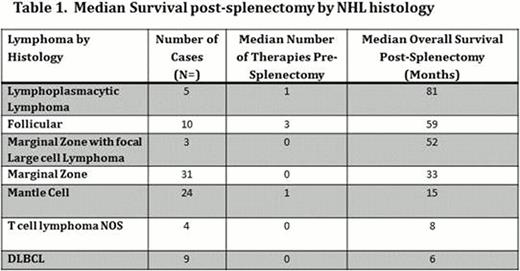
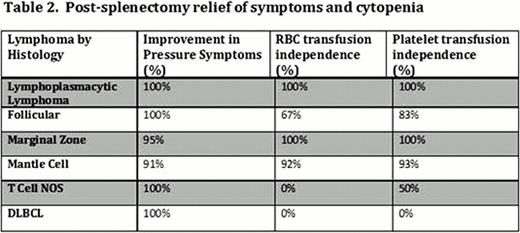
Median age at splenectomy was 67 years (range 42–84 yrs.) and 56 (62%) of patients were male. Average time from diagnosis to splenectomy was 3 months (range 0–217 months). Splenectomy was the first treatment in 56 (62%) patients; the other 34 patients were treated with chemotherapy with an average of two previous regimens. Most patients had involvement outside of the spleen, 65 (72%) with concurrent bone marrow involvement and 35 (50%) with lymph node involvement. Various different NHL histologies were represented: marginal zone (MZ) (34%), mantle cell (MC) (26%), diffuse large B-cell lymphoma (DLBCL) (10%), follicular (FL) (11%), lymphoplasmacytic (LP) (6%) and T cell NOS (4%). With a median follow-up time of 25 months, the median overall survival differed by histology type of NHL (Table 1). Indolent lymphomas such as FL, LP and MZ had more favorable survival compared with more aggressive lymphomas such as DLBCL and T cell NOS. Splenectomy was safe and well tolerated with only one treatment related death. There were no reported post-splenectomy septic events. Two patients did develop a portal vein thrombosis. 95% of patients had relief in pressure and abdominal symptoms post-splenectomy. With the exception of patients with DLBCL and T-cell NHL, a majority of patients had improvement in anemia and thrombocytopenia related to splenomegaly (Table 2).
This represents the largest reported series of patients with lymphoma treated with splenectomy. Our results indicate that median overall survival after splenectomy is determined by the underlying type of NHL. Patients with LP, FL, MZ and MCL have a favorable outcomes following splenectomy. Splenectomy remains a safe and effective treatment option for massive splenomegaly in selected patients during the course of their disease management.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal