Abstract
Abstract 2685
Genetic alterations such as C-MYC, BCL2, BCL6 translocations and TP53 alterations have a prognostic impact in patients with aggressive B-cell lymphomas (Johnson et al JCO 2012; Sietse et al Blood 2011; Young et al Blood 2009). Here we provide novel information about the influence on survival of sole C-MYC translocation compared with additional BCL2 and/or TP53 alterations. The clinical outcome of 28 patients with C-MYC positive diffuse large B-cell lymphoma (DLBCL) (N=4) or B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and Burkitt lymphoma (B-UNC/DLBCL/BL) (N=24) was retrospectively evaluated according to their genetic alterations (GA) and therapy (R-CHOP N=10 (36%) patients vs. B-ALL-GMALL containing HD-MTX, N=18 (64%) patients). C-MYC, BCL2 and TP53 alterations were screened by FISH. TP53 mutations were investigated by immunohistochemistry, positive cases were further sequenced. Cases were grouped in 4 categories: C-MYC only (32%), C-MYC & BCL2 (32%), C-MYC & TP53 (21%) and triple hit (14%). Statistical analyses were performed using R for Windows 2.12.1 (R Development Core Team) software. P-values < 0.05 were considered as significant.
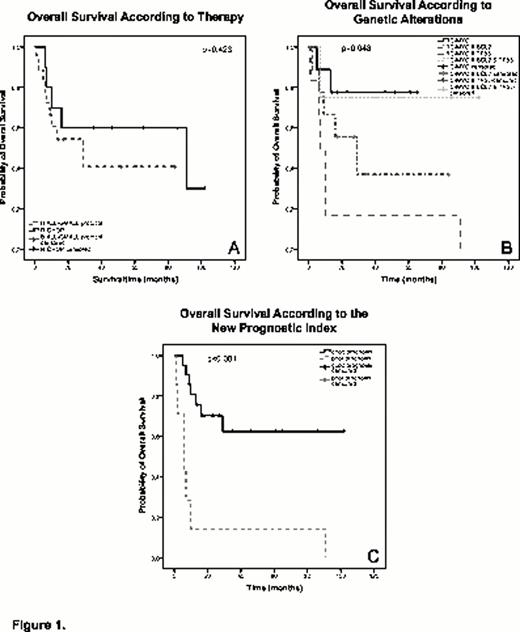
Using Kaplan Meier survival analysis no significant difference was found between therapeutic regiments indicating no advantage for aggressive chemotherapy (Fig. 1A). Based on the GA overall survival (OS) was significantly different between the four groups (p=0.048). OS at five years was 75% for C-MYC, 71% for triple hit, 35% for C-MYC & BCL2 and 17% for C-MYC & TP53 (Fig. 1B). These data confirm previous results in MYC-induced murine lymphomas (Schuster et al Blood 2011). In the log-rank test only low International Prognostic Index (IPI) scores (0–1) predicted survival correctly. Due to this fact, we aimed to define a new prognostic index containing genetic parameters.
Univariate and multivariate analyses were performed to identify predictive parameters. Patient characteristics were tested for potential influence on OS using the Cox proportional hazards model in combination with all-possible-subset regression. Covariates were: age, LDH (U/ml), BM infiltration (%) and factor variables: sex, LDH high vs. low, presence or absence of BM infiltration, localization (extranodal vs. nodal), clinical stage, IPI-score, therapy and GA. Model selection was performed using the all-possible subset approach, calculating all models with j=1 to 11 covariates. A model was considered valid if all predictors exhibit p-values below 0.05. A factor variable was considered significant if at least one level differs significantly from a predefined base level (base level for GA: sole C-MYC; therapy: GMALL-ALL protocol; stage: CS I; IPI: 0 points). The final model was checked for possible evidence of non-proportional hazards and for influential observations. Table 1. shows the characteristics of the multivariate Cox regression model including the covariates BM and GA (explained variation R2=0.48).
Model characteristics for the two-variable model containing genetic alterations and BM infiltration as significant covariates.
| Covariate/factor level . | Regression coefficient βj . | Relative Risk exp(βj) . | p-value . | 95 % Confidence Interval . |
|---|---|---|---|---|
| C-MYC & BCL2 | 2.8 | 16.7 | 0.008 | [2.1; 135] |
| C-MYC & TP53 | 4.3 | 71.4 | < 0.001 | [5.6; 904] |
| C-MYC & BCL2 & TP53 | 0.2 | 0.8 | 0.87 | [0.07; 9.1] |
| BM | 3.2 | 25.0 | 0.001 | [3.5; 178] |
| Covariate/factor level . | Regression coefficient βj . | Relative Risk exp(βj) . | p-value . | 95 % Confidence Interval . |
|---|---|---|---|---|
| C-MYC & BCL2 | 2.8 | 16.7 | 0.008 | [2.1; 135] |
| C-MYC & TP53 | 4.3 | 71.4 | < 0.001 | [5.6; 904] |
| C-MYC & BCL2 & TP53 | 0.2 | 0.8 | 0.87 | [0.07; 9.1] |
| BM | 3.2 | 25.0 | 0.001 | [3.5; 178] |
It became obvious that the presence of C-MYC & BCL2 or C-MYC & TP53 increased the relative risk for lymphoma related death whereas C-MYC only and interestingly also triple hit cases showed favorable prognosis in this rare entity. These finding motivated the definition of a new prognostic index: assigning one point each to the risk factors 1) BM infiltration, 2) C-MYC & BCL2; two points to 3) C-MYC & TP53 and no point to 4) presence of sole C-MYC or 5) triple hit aberrations, respectively, yielding scores between 0 and 3. Based on these scores two prognostic groups “good” (scores 0–1) vs. “poor” (score 2–3) were classified. OS stratified by the new risk groups was highly significant (p-value < 0.001) (Fig. 1C).
Our data indicate that 1) C-MYC and TP53 simultaneous alterations constitute the highest risk group. This risk is considerably ameliorated when an additional BCL2 aberration is present. 2) GMALL-ALL protocol is non-superior to R-CHOP. 3) Our prognostic index integrating clinical and genetic features is able to predict outcome and should be evaluated in larger studies.
Jaeger:Emergent Product Development: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal