Abstract
Abstract 2673
Follicular Lymphoma International Prognostic Index 2 (FLIPI-2) is a widely accepted tool for risk assessment of follicular lymphoma (FL), which is based on age, hemoglobin level, presence of bone marrow (BM) invasion, tumor size, and b2-microgloblin levels. Although it is easy to evaluate in clinical practice, it is a combination of tumor burden and patient physical condition, and a simple and powerful biomarker reflecting the tumor burden and its character is still not established. LR11 (also called SorLA or SORL1) was identified and characterized as a regulator of uPAR function through complex formation with uPAR. We have identified that serum soluble LR11 (sLR11) levels are significantly elevated in patients with acute leukemia and B cell lymphomas, and are associated with tumor burden and BM invasion (Sakai et al 2012). We have also found that high sLR11 levels had a significant negative prognostic impact on progression-free survival (PFS) in FL. Therefore, we have retrospectively evaluated the clinical characteristics of sLR11 and its prognostic impact on FL, in a larger patient cohort.
Sixty-one patients with FL treated at Chiba University Hospital and affiliated hospitals from 2002 to 2012 were evaluated. The majority of patients were treated by the R-CHOP regimen (rituximab 375 mg/m2 on day 1; cyclophosphamide, 750 mg/m2 on day 1; adriamycin, 50 mg/m2 on day 1; vincristine, 1.4 mg/m2 on day 1; and prednisolone, 100 mg/body on day 1–5). Serum sLR11 levels were measured by ELISA method. Patient laboratory data and treatment outcome were obtained retrospectively.
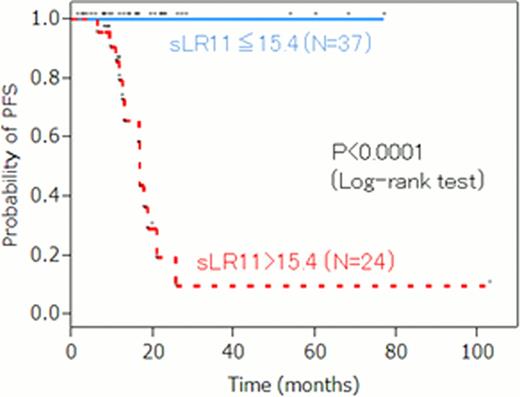
Serum sLR11 levels of patients with lymphoma were significantly increased (mean ± SD: 19.4 ± 17.1 ng/ml) compared with those of normal control subjects (8.8 ± 1.79 ng/ml, P<0.0001). Paired sample analysis at diagnosis and at remission showed significant reduction of sLR11 levels at disease remission (22.0 ± 23.9 ng/ml vs. 8.1 ± 3.0 ng/ml, P<0.0001). Multiple stepwise linear regression analysis showed that the serum sLR11 level at diagnosis was independently associated with BM invasion, lower Hb levels and elevated b2-microglobulin levels (r2= 0.48, BM invasion: P=0.0333, lower Hb levels: 0.0004, elevated b2-microglobulin levels: P=0.0289). Patients with “high” FLIPI-2 score showed significantly higher sLR11, compared to those with “intermediate” and “low” FLIPI-2 scores (29.2 ± 5.1 vs. 13.8 ± 7.7 ng/ml, p<0.0001). The receiver operating characteristic curve analysis showed that the cut off level of 15.4 ng/ml provided a maximum sensitivity (0.86) and specificity (0.82) for “high” FLIPI-2 score; the area under the curve was 0.84. At the median follow-up period of 15.7 months, the probability of 5-year PFS was significantly higher in patients with sLR11 >15.4 ng/ml at diagnosis compared with those with ≤15.4 ng/ml (Figure 1, 9.7 % vs 100 %, P<0.0001). Cox regression analysis showed that serum sLR11 levels >15.4 ng/ml at diagnosis was a significant prognostic factor for PFS (hazard ratio: 2.65 × 107, 95% CI: NA).
Serum sLR11 levels in FL patients were associated with BM invasion, lower Hb levels and elevated b2-microglobulin, which are 3 of 5 variables in FLIPI-2. This suggests that serum sLR11 is a useful tool to predict “high” FLIPI-2 score, especially highlighting those with high tumor burden by simple serum evaluation and can be a promising biomarker in patients with FL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal