Abstract
Abstract 2651
In non-Hodgkin lymphoma (NHL), individual characteristics of the tumor cells alone are not the only parameters which determine prognosis and overall survival. Non-malignant immune cells and the tumor microenvironment also play an important contributory role in determining the eventual clinical outcome. There is an increasingly growing interest in the role of monocytes and their precursors in the pathogenesis of lymphoproliferative disorders. Recently, elevated peripheral blood monocyte counts have been shown to be an independent prognostic parameter associated with poor prognosis and decreased overall survival in patients with both non- Hodgkin lymphoma and Hodgkin. The main aim of this collaborative multicenter study was to re-evaluate and attempt to verify the prognostic significance of monocytosis (> 800 cells/mm3) at diagnosis, in a large cohort of 1026 newly diagnosed patients with diffuse large B-cell lymphoma (DLBCL) followed at different medical centers both in Israel and Italy. Additional aims of this study were to define possible correlations with a number of other well recognized prognostic factors in DLBCL.
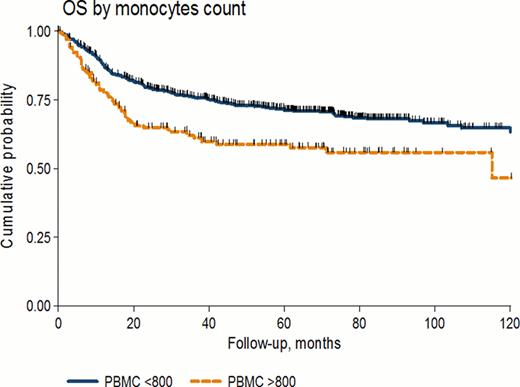
We reviewed clinical and laboratory data of consecutive untreated patients with DLBCL, followed and eventually treated in different centers in Haifa, Israel and in Italy between 1993–2010. Median age at diagnosis was 59 years (range 18–95 yrs) and the 5-years OS after a median follow up of 51 months (range 0.2–180 months) was 69% for the entire cohort. Monocyte counts were available for 852 patients. Those with peripheral blood monocyte count (PBMC) < 800 mm3 had a 5 years OS of 71%, compared to 59% for those with PBMC > 800 mm3 (p=0.0002). In univariate analysis age, IPI score and monocyte counts were associated with a worse OS. In multivariate analysis, monocytosis retained a negative prognostic value even when adjusted for IPI (HR 1.53, CI95% 1.16–2.02, p=0.003).
Of the 852 patients, 496 (58%) were treated with chemotherapy alone, while 356 patients (42%) received chemo-immunotherapy with similar regimens including rituximab. The addition of rituximab to the combination chemotherapy did not abrogate the negative adverse effect of monocytosis (p=0.0015) observed in patients receiving chemotherapy alone.
This large validation study confirms earlier very recent results and shows that the monocyte level (monocytosis), a simple prognostic parameter, can easily be used routinely to evaluate newly diagnosed patients with DLBCL and identify those with a higher risk of poor survival. The addition of monocytosis as an additional parameter to the basic IPI, may possibly generate a more comprehensive score incorporating both patient, tumor and immune parameters.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal