Abstract
Abstract 2639
A variety of secondary malignancies have been observed among patients treated for Hodgkin lymphoma (HL) including non-Hodgkin lymphomas (NHL). Data on risk of developing NHL after therapy for HL is limited. The management of patients with secondary (after HL) NHL (sNHL) may be challenging due to the cumulated toxicity from HL treatment. The outcome of patients with s NHL relative to their de novo counterparts (dn NHL) is unknown.
We used data from the National Cancer Institute's Surveillance Epidemiology and End Results (SEER-18) to determine the incidence and long term overall survival (OS) of patients with secondary NHL (sNHL) after HL therapy. Inclusion criterion was diagnosis of HL in the period of 1992–2009 as first malignant neoplasm. To avoid inclusion of patients with concomitant HL and NHL diagnosis, cases with the two distinct histologies reported up to 3 months apart as well as patients with HL and less than 3 months of follow up were excluded from the analysis. Follow up was updated up to the end of 2009 (November 2011 submission). Cumulative incidence of sNHL among HL survivors was calculated using a competing risk model, treating death from any cause in absence of sNHL as the competing risk. In order to compare outcomes of sNHL with dnNHL, we matched dnNHL to sNHL cases in a 2:1 ratio based on the following parameters in decreasing priority: histological subtype, stage, calendar year of diagnosis, age, race, gender, and SEER registry. A Cox proportional hazard model with normal frailty was used to compare OS of sNHL cases to the dnNHL cases.
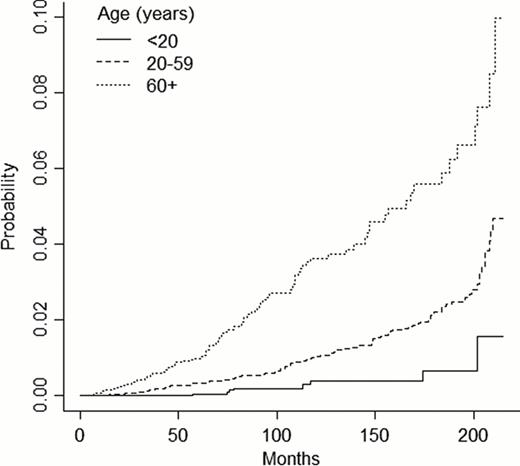
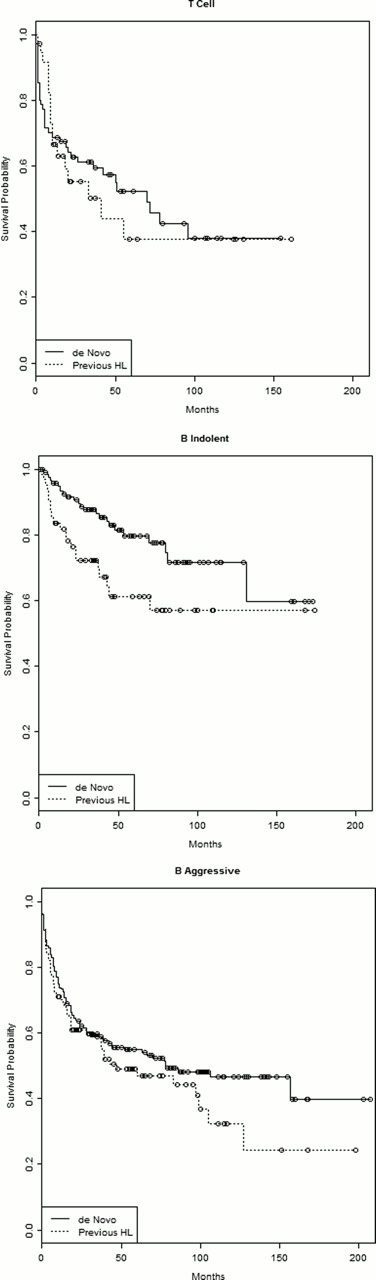
A total of 26,826 HL cases were included in the analysis with median follow up of 62 months (range 3–215). Median age of patients was 34 years (range 2–99), 8324 (31.0%) had advanced stage, 14619 (54.5%) had limited stage and stage was unknown for 3883 (14.5%) patients. The cumulative incidence of sNHL was 0.41% (95% C.I. 0.32–0.50), 1.34% (95% C.I. 1.41–1.55) and 2.50% (95% C.I. 2.10–2.89) 5 years, 10 years and 15 years after the diagnosis of HL respectively. Incidence of sNHL was closely linked to age at diagnosis of HL. Cumulative incidence at 15 years post HL diagnosis was 0.67% (95% C.I. 0.04–1.29) for age <20 years, 2.23% (95% C.I. 1.77–2.67) for age 20–59 years and 5.59% (95% C.I. 4.21–6.97) for age 60 or older (p<0.001, Figure 1). Overall, 259 cases of sNHL were diagnosed. Most patients with sNHL were males (62.2%) and white (84.6%). The median age at the diagnosis of sNHL was 56 years (range 10–92). Thirty eight (14.7%) sNHL were T-cell lymphomas, 144 (55.6%) aggressive B-NHL, 64 (24.7%) indolent B-NHL and 13 (5%) were not classified. Patients with sNHL had worse OS than their dnNHL counterparts for indolent B-NHL (HR of death 2.7, 95% CI 1.3–5.7, p=0.008) but not for aggressive B-NHL (HR 1.3, 95% C.I. 0.6–2.7, p=0.19) or T-NHL (HR 0.8, 95% C.I 0.3–1.8, p=0.42). Overall survival per histological group is displayed in Figure 2.
The risk of developing sNHL after therapy for HL is substantial, particularly among older patients. The OS for patients with indolent B-cell sNHL is inferior to their matched dnNHL counterpart. Such difference in outcome could not be verified for aggressive B-cell and T-cell sNHL
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal