Abstract
Patients with acute leukemia and in particular, patients with acute promyelocytic leukemia (APL), are considered to be at high risk for the development of venous thromboembolism. The presence of central venous catheters (CVC) increases the risk of thrombotic complications; however, previous reports have varied as to the frequency of this complication. Current guidelines do not recommend the routine use of prophylactic anticoagulation for patients with CVC.
We have suspected an increased incidence of CVC thrombosis in patients with APL and therefore conducted a retrospective survey of 473 patients who were treated for acute leukemia at our institution.
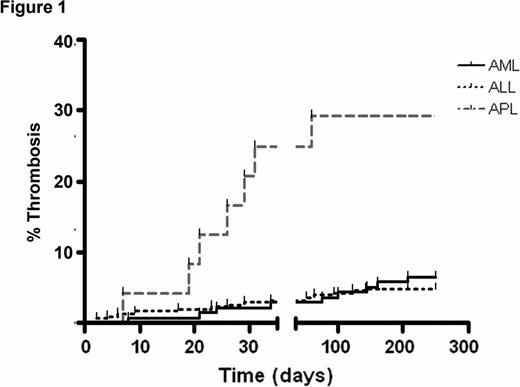
The overall rate of symptomatic CVC thrombosis was 6.8%. We found a significantly (p< 0.001) increased rate of symptomatic CVC thrombosis (32%) in patients with APL as compared with patients with acute lymphocytic leukemia (ALL) and acute myeloid leukemia (AML) (6.4% and 4% respectively) as shown in Figure 1. CVC thrombosis was most prevalent following induction treatment, during the period of recovery of blood counts, and was associated with significantly higher platelet counts in patients with APL compared to other AML patients. We therefore relate this higher thrombosis rate to the disease pro-coagulants, the treatment with all-trans-retinoic-acid and the high platelet counts at the time of induction recovery.
Subsequently, following this observation, we treated 13 newly diagnosed patients with APL with low molecular weight heparin prophylaxis during the induction recovery phase of blood counts. None of these patients had a thrombotic event, nor a bleeding complication.
Although our treatment group was small, we suggest considering prophylaxis for CVC thrombosis during platelet recovery after induction treatment in patients with APL.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal