Abstract
Abstract 2465
This study was designed to identify single nucleotide polymorphisms (SNPs) associated with probability of achieving a major molecular response (MMR) in chronic phase CML patients (pts) treated with imatinib. We used a non-commercial, pharmacogenetics-dedicated DNA chip containing 16561 SNPs covering 1916 candidate genes. We tested an exploratory cohort of pts treated with imatinib first line or after interferon therapy and then extended our finding in a validation set of pts included in the French SPIRIT trial (C Preudhomme, NEJM 2011) and randomized to the 400 mg or the 600 mg imatinib arm.
Constitutive DNA samples from 312 pts were analyzed: samples from 91 pts in the exploratory set and 221 pts in the validation set (SPIRIT trial: 120 pts within the 400 mg imatinib arm and 101 pts within the 600 mg imatinib arm). We analyzed the expression of BCR-ABL/ABL standardized ratio as a function of the time elapsed since imatinib initiation for each patient using nonlinear (spline) interpolation and then derived the delay to achieve MMR or time of follow-up. With this method, we obtained a cumulative incidence curve of MMR in both groups. Relevant SNPs were identified using a COX model adjusted for covariates (sex, two first principal components and Sokal score when available). SNP with FDR (False Discovery Rate) below 30% in the exploratory cohort where subsequently investigate in the SPIRIT trial groups.
Patient characteristics such as age, sex, Sokal score were homogeneous between exploratory and validations sets as well as within both arms of the SPIRIT trial. We confirmed the prognostic value of the Sokal score in term of cumulative incidence of MMR (CI-MMR) in both sets of pts (CI-MMR was 83%, 67% and 56% for low, intermediate and hight Sokal risk groups respectively, additive log rank, p < 0.001), as well as the significant improvement of CI-MMR within the SPIRIT trial for pts assigned to the 600 mg daily imatinib arm as compared to the 400 mg daily arm (CI-MMR was 80% in the 600 mg imatinib arm compared to 61% in 400 mg/day arm, log rank, p = 0.008). CI-MMR was similar between exploratory set and the 400 mg/day arm of the SPIRIT trial (63% vs 61%, log rank, p = 0.56) and higher in the 600 mg arm of the SPIRIT trial compared to the exploratory set: 80% vs 63% (log rank, p < 0.001), consistent with dose received in the exploratory set (imatinib 400 mg/d).
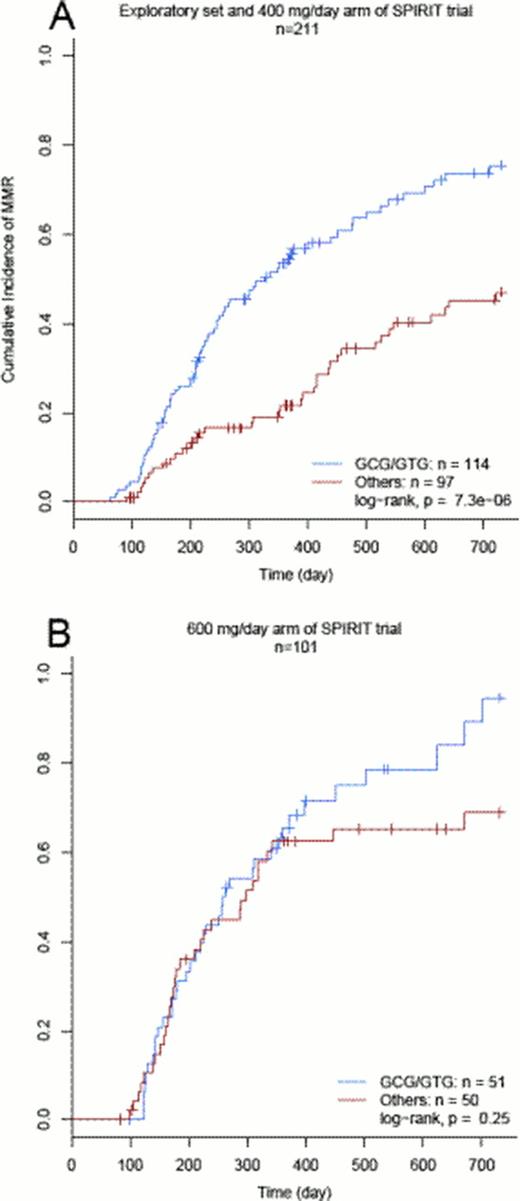
Association study shows that 10 SNPs identified pts with significantly different probability to achieve MMR within the two first year of therapy (FDR less than 30% p < 0,01) in the exploratory cohort three of which belong to ABCG2 gene. In the SPIRIT trial (n=221), only two SNPs from ABCG2 locus were significantly associated with a higher probability of achieving MMR. We then analyzed separately both arms of the SPIRIT trial. All tree ABCG2-SNPs identified in the exploratory set of pts were significantly associated with CI-MMR in the 400 arm at the 5% level. In contrast, none of them were confirmed in the 600 mg arm. In order generalize our results and to get closer to the underling molecular structure of genotypes markers we performed haplotyping at locus of ABCG2 gene. Multivariate analysis distinguished two minor haplotypes (haplotype 1 and 3) linked to MMR achievement in pts receiving 400 mg/day of imatinib (from exploratory set and SPIRIT, n=211). Haplotypes 1 had G-C-G and haplotype 2 had G-T-G at rs12505410, rs13120400 and rs2725252 respectively and their frequencies were 26 and 6% respectively. Collapsing these haplotypes yielded a surrogate dominant marker highly associated to CI-MMR in this group (p < 0.001, figure 1A) whereas in the SPIRIT 600 mg arm, this phenomenon did not hold anymore (p=0.25, figure 1B). Interestingly, CI-MMR in the 400 mg/day harboring a copy of minor haplotypes (1 or 3) was comparable to the CI-MMR observed in pts receiving 600 mg/d imatinib lacking of at least one copy of the two minor haplotypes (75% vs 70% respectively, p=0.99) or whatever haplotype they had (75% vs 80%, p=0.37).
The ABCG2 gene product is a well-known protein involved in drug absorption in the bowel. Polymorphism of the ABCG2 gene has been implicated in drugs absorption including imatinib. We here confirm that ABCG2 haplotypes could distinguish patients at a lower probability to achieve MMR. We report for the first time that this unfavorable pharmacologic effect can be overcome in vivo by increasing imatinib daily dose from 400 mg to 600 mg.
Rousselot:BMS, Novartis: Research Funding. Guilhot:ARIAD: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal