Abstract
Sickle cell disease (SCD) is the most common inherited blood disorder caused by a mutation in the beta-globin chain of the hemoglobin (Hb) molecule. The result of this mutation, Hb S, polymerizes when deoxygenated, giving the red blood cells a characteristic, sickled shape. This polymerization causes in vivo vaso-occlusion and disrupts the vascular endothelium causing multi-organ complications in affected individuals. Nearly 70% of all affected births occur in Africa, where conservative estimates of SCD prevalence suggest a 10.68/1000 rate at birth (compared to 0.49/1000 in the U.S.). Although SCD causes significant morbidity and premature mortality, most affected persons born in the U.S. are able to survive into adulthood (primarily due to the implementation of universal newborn screening). In contrast, most affected individuals born in low-income countries die before the age of 5 years due to lack of early intervention. Current technology for diagnosing SCD relies on hemoglobin electrophoresis, isoelectric focusing or high performance liquid chromatography. This type of testing remains prohibitively expensive to low-income countries, where SCD is most prevalent and newborn screening is unavailable. Thus, many affected individuals are not diagnosed before severe complications or death can occur. The urgent need to develop a low-cost diagnostic test for SCD has been recently recognized as a priority by the World Health Organization. In this study, we describe the implementation of a paper-based hemoglobin solubility assay as a simple, low-cost and rapid test for definitive diagnosis of SCD.
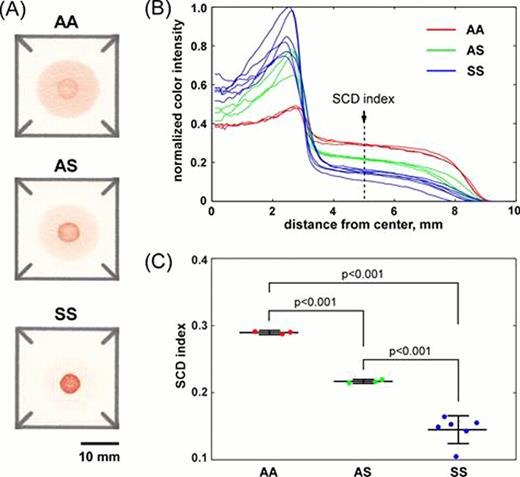
Normal human venous blood (Hb AA) was collected and compared to blood from patients with SCD (Hb SS) and SCT (Hb AS). To perform the test, a 20uL droplet of whole blood mixed with the components of the Hb solubility assay (SickleDex™, Streck) was deposited onto a paper-fluidic device fabricated using a previously published method. Polymerized deoxy-Hb S remained in the center of the blood stain entrapped by the paper substrate, while other forms of Hb remained soluble and were transported laterally to the periphery of the stain by capillary action. The resulting blood stain was digitized with a portable scanner and analyzed automatically. The red color intensity profiles were normalized by the total area under the curve to account for the differences in hematocrit among subjects. The SCD index was defined as the normalized color intensity 5 mm from the center of the blood stain. Data were presented as results of individual experiments and as mean ± SD. The values of the SCD index for samples from each Hb genotype were compared using a paired two-tailed t-test.
The entanglement of polymerized deoxy-Hb S by the fibers of the paper substrate resulted in the formation of a dark red spot in the center of the blood stain, while the wicking of the soluble forms of Hb from the center produced a pink ring on the periphery of the stain. The patterns of the blood stains produced on paper by normal (Hb AA), SCT (Hb AS) and SCD (Hb SS) samples were significantly different (Fig. A). The tight clustering of the normalized color intensity profiles for different subjects with the same Hb genotype enabled the use of the SCD index as a quantitative metric for distinguishing between the three types of samples (Fig. B). The difference between the SCD index measured for Hb AA, Hb AS and Hb SS samples was highly significant, with p<0.001 (Fig. C). Unlike the conventional, commercially available Hb solubility tests (e.g. SickleDex), the paper-based Hb solubility assay can conclusively differentiate between SCT and SCD samples using the characteristic blood stain patterns produced by each sample on the paper substrate.
This proof-of-concept study demonstrated the feasibility of using the paper-based Hb solubility assay as a simple, low-cost, point-of-care diagnostic test for SCD. The ability to diagnose SCD quickly and inexpensively will be particularly useful for universal SCD screening in resource-limited settings, such as Africa. This test will also be very useful in the emergency room setting in high-income countries to enable healthcare professionals to objectively confirm suspected SCD at the bedside.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal