Abstract
Susceptibility to encapsulated bacteria, particularly Streptococcus pneumonia, is well known in sickle cell disease (SCD). Hydroxyurea (HU) is commonly used in adults and children with SCD, but, little is known about the effects of HU on immune function in SCD and recommendations for immunization are lacking. As HU reversibly inhibits ribonucleotide reductase, causing cell cycle arrest at the G1-S interface, we postulated that HU might delay the transition from naïve to memory T cells, resulting in a delay in immunologic maturation, with deleterious effects on vaccine responses; therefore, T cell subsets, including conversion of naïve to memory T cells and antibody (Ab) responses to pneumococcal (Pnu), measles, mumps and rubella (MMR) vaccinations were studied during the BABY HUG Trial of HU for infants and toddlers with SCD.
Blood was collected for measurement of: T cell subsets at entry (9–18 mos of age), age 24 mo and exit after 2 yrs of treatment; Pnu Ab levels were measured (by EIA after preabsorption with C-polysaccharide) at entry, before and 2–8 wks after 23-valent polysaccharide (PS) PCV23 vaccine at age 24 mo, and exit; and MMR antibodies at entry, 1–10 weeks after MMR at age 12 mo, age 24 mo and exit.
Of the 193 subjects in BABY HUG, T cell subsets were available for 91 HU and 88 placebo (PL) subjects. At entry, there were no significant differences in absolute lymphocyte count (ALC), or % or absolute T cell subsets between the HU and PL groups. At age 24 mo, both groups had an age-related decline in ALC, with significant differences between the HU and PL groups in ALC (5740 vs. 7323/mm3; p=0.003), absolute CD4 cells (1912 vs. 2247/mm3; p=0.022) and memory CD4 cells (392 vs. 487/mm3; p=0.003). The same pattern was seen at exit for ALC (4836 vs. 5764/mm3; p=0.015), absolute CD4 cells (1510 vs. 1747/mm3; p=0.043) and memory CD4 cells (360 vs. 444/mm3; p=0.003).
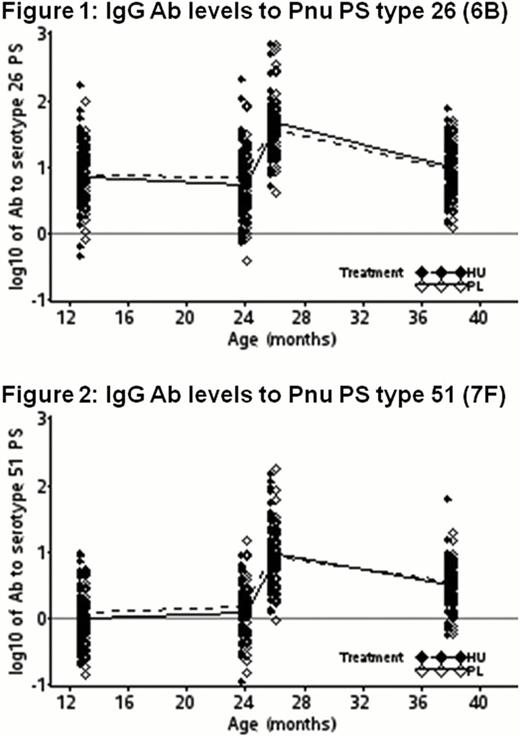
IgG Ab levels to Pnu antigens were measured at entry [after 3 doses of PS/protein conjugate (PC) PCV7 containing Pnu PS type 26 (6B), but not 51 (7F)], before and after immunization with PS PCV23 vaccine at 24 mo, and at exit, with no significant differences between the HU and PL groups in mean Ab levels at any time point for either serotype (Fig 1&2).
For those immunized with MMR prior to study treatment, there were no differences in % immune for measles, mumps, or rubella between the HU and PL groups at any time point. For 40 HU and 38 PL subjects immunized after starting study treatment, there was a smaller % of HU-treated children with protective response to measles vaccine 1 – 10 wks after immunization [HU 71.4% (10/14) vs. PL 100% (24/24); p=0.014]. Response to mumps [HU 78.6% (11/14) vs. PL 91.7% (22/24)] and rubella [HU 66.7% (10/15) vs. PL 92% (23/25)] vaccines showed similar trends, but no statistical significance. The HU vs. PL difference in failure of response to at least one vaccine virus was of similar significance (p = 0.021) to that of measles alone. By age 24 mo, there were no significant differences in response to MMR (89.7 to 100%). Mean Ab levels to measles and rubella were also significantly lower in the HU group 1–10 wks after immunization (p=0.005 and p=0.011, respectively).
HU given to infants and young children with SCD causes a reduction in ALC, CD4 T cell and memory T cell counts. Additional monitoring of HU-treated children with SCD for these and related T cell parameters is warranted until the biological effects on immunity are known with certainty.
Response to Pnu vaccine was not affected by HU therapy, suggesting that there is no increased risk for Pnu sepsis in infants and children with SCD treated with HU, consistent with the clinical results in the BABY HUG trial.
Although the sample was small, a delay in achieving protective measles Ab levels was seen in the HU group, and possibly for mumps and rubella. This delay cannot be estimated precisely, due to study design, but Ab levels to all 3 viruses were similar at exit, indicating that effective immunization can be achieved despite HU use. For endemic or local epidemics of measles, mumps, rubella or other pathogens requiring immunization, adherence to recommended accelerated immunization schedules will be especially important for children with SCD treated with HU.
Off Label Use: Off-label use of hydroxyurea in infants and children. Casella:Adventrx: Consultancy, Research Funding.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal