Abstract
Abstract 2171
Post operative bleeding is a common complication of cardiac surgery; its aetiology may be multifactorial but is often attributed to platelet dysfunction. However, at present no reliable point of care test (POCT) is available for this and patients are often managed empirically; approximately 40% receive pooled platelet transfusions but many require re-sternotomy. An automated microchip flow chamber system that directly measures platelet-collagen interaction under shear (1500s−1) has recently been developed (T-TAS; Total Thrombus-formation system; Zakros, Fujmori Kogyto, Japan). We hypothesized that this could be developed as a POCT to assess platelet function under shear, allowing targeted and more rational use of blood products. We used this system to study 20 patients aged 19–72 years, before and after cardiac surgery. The T-TAS was used to determine the onset of occlusion (time to 10kPa, T10) and primary haemostatic potential (AUCend-area under pressure curve). Haematocrit (Hct), platelet count and von Willebrand factor (VWF) levels and thromboelastography (TEG) were measured at the corresponding time points.
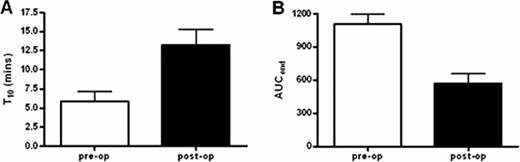
Surgery resulted in a significant increase in time to occlusion onset (T10) (p=0.006; n=20, Figure 1A). Similarly, the AUCend significantly decreased after surgery (p=0.001, n=19; Figure 1B) with the majority of cases (12 out of 20) failing to occlude within 30 minutes. The change in T10 inversely correlated with change in AUCend(r=-0.5, p=0.02).
VWF is essential for platelet adhesion to collagen under high shear stress. Higher VWF levels appeared to be associated with lower T10, but this was not significant and only observed prior to surgery. Moreover, no significant correlation between the change in T10 or AUCend and changes in VWF pre- and post-surgery was observed.
Surprisingly, pre and post-operative hematocrit were both negatively correlated with AUCend (r=-0.5, p=0.03, n=11 and r=-0.5, p=0.02,n=11 respectively).
No correlation was observed between platelet count and the T-TAS parameters. However, the change in AUCend (but not T10) was shown to correlate with the change in platelet count before and after surgery (r = 0.58, p = 0.01).
Finally, T10 and AUCend values were not significantly altered in patients given anti-platelet drugs: aspirin and/or clopidrogel. This implies that the T-TAS is sensitive to the initial adhesion of platelets to VWF-collagen rather than to platelet activation and aggregation.
These data demonstrate that cardiac bypass surgery affects VWF mediated platelet adhesion to collagen under flow and this can be detected using a microchip flow chamber system. The lack of correlation with VWF levels and apparently paradoxical effect of haematocrit suggest that the dominant mechanism for the impaired postoperative haemostasis is a decline in platelet function and in particular a decrease in adhesive function. This is likely to result from altered exposure and/or function of GPIb resulting from surgery and cardio-pulmonary bypass.
Current POCTs are largely insensitive to primary haemostatic mechanisms, while conventional laboratory measures of primary haemostasis are non-physiological, and require a considerable expertise and time. As expected, TEG gave similar values pre and post-surgery for all subjects, indicating that a flow system is required to adequately evaluate primary haemostasis. The advantages of this novel automated microchip flow chamber system are the small blood volume required and the rapidity of results. Our data suggest a place for this system in a point-of care setting, providing useful assessment of haemostatic status following surgery and with the potential to improve patient management. Further studies are warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal