Abstract
Abstract 2067
Pneumococcal invasive infections are over 13 times more common among patients with hematological malignancies than in the general population. Hematopoietic stem cell transplant (HSCT) recipients, particularly those with chronic graft-versus-host disease (cGvHD), are especially vulnerable.
Two types of vaccines are available for prevention: pneumococcal polysaccharide vaccine (PPSV) and pneumococcal conjugate vaccine (PCV). PPSV covers more serotypes, but concerns have been raised over immune response, particularly in immunocompromised patients.
The primary goals of this study were to evaluate clinical impact of pneumococcal bacteremia, serotypes involved and resistance profile in our hematological population.
We performed a retrospective study based at Hôpital Maisonneuve-Rosemont and Hôpital Notre-Dame du CHUM, both in Montreal, Canada. Among all positive blood cultures for Streptococcus pneumoniae between January 1st, 2003 and December 31st, 2011, we selected patients with hematological malignancies. We reviewed patients' charts and electronic files. Serotypes and antibiotic susceptibility testing were done by the Laboratoire de Santé Publique du Québec. The study was approved by the hospitals' ethics committee.
During the eight-year period, 54 episodes of pneumococcal bacteremia (in 52 patients) occurred among patients with hematological malignancies. Median age was 63.5 years (range 21 to 91); 44% were female. One patient was splenectomized.
The main hematological malignancies were multiple myeloma (42%) and non-Hodgkin lymphoma (29%). There were 16 HSCT recipients: 10 allogeneic (8 with cGVHD) and 6 autologous. Twenty-nine patients (55%) were on chemotherapy, including 10 HSCT recipients. Among the patients with cGVHD, 3 were on trimethoprim-sulfamethoxazole (TMP-SMX) prophylaxis and 1 on pentamidine.
At the time of the bacteremia, 81% of patients had a diagnosis of pneumonia (mean Fine score 118. Eleven patients were treated in the emergency department or in the outpatient clinic. Among the 43 hospitalized patients (80%), median hospitalization duration was 10 days. Intensive care unit admission was required for 9 episodes (17%). Eight patients died less than 30 days after the diagnosis of bacteremia, leading to a mortality rate of 15% and 19% among HSCT recipients.
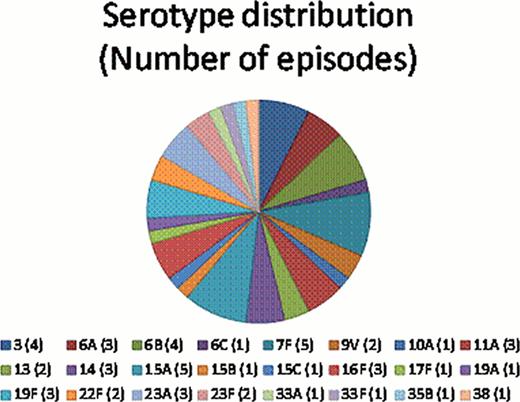
Vaccine history was not available in most patients' charts. However, all HSCT recipients should have received PPSV, as recommended in our institution. Twenty-four different serotypes were found. Theoretical coverage of these serotypes by the available vaccines was 26% for PCV-7, 35% for PCV-10, 50% for PCV-13, and 61% by PPSV; 33% episodes were not covered by any vaccine. Among patients with HSCT, the percentage of episodes not covered by any vaccine increased to 44%. PPSV covered 56% of episodes.
Resistance to TMP-SMX was found in 17% of isolates. However, since 2006, all were susceptible. A third of isolates were resistant to erythromycin; the proportion of resistant isolates was higher among HSCT patients (50%). Only one isolate was resistant to fluoroquinolones, but was sensitive to all other antibiotics tested. One strain was of intermediate sensitivity to ceftriaxone, and was resistant to erythromycin and TMP-SMX. This patient was on TMP-SMX prophylaxis, and did not require admission. All strains were sensitive to penicillin and vancomycin.
Pneumococcal bacteremia carries significant morbidity and mortality in patients with hematologic malignancies. Our mortality rate is similar to that found in other studies. Vaccination remains the cornerstone of prevention, but is imperfect in terms of immune response and coverage. One third of episodes were not covered by any available vaccine, and this proportion increased among HSCT recipients. Antibacterial prophylaxis in patients with cGVHD is therefore important and penicillin remains a good choice.
In terms of treatment options for respiratory infection, given the high erythromycin resistance rate (34% vs. 20–25% found in the general population), macrolides should not be used as single agents. Third generation cephalosporins and fluoroquinolone resistance is very low, making it an interesting choices for respiratory infections.
Labbé:Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal