Abstract
Abstract 2062
We and others have noted that venous thromboembolism (VTE) is a common complication of hematopoietic stem cell transplant (HSCT). However, bleeding complications are even more common. Consequently, our center takes a cautious approach to VTE prevention. The purpose of this study was to determine VTE prophylaxis practice patterns among providers caring for patients during HSCT.
We generated a 20 question web-based survey to determine institutional VTE prevention practices. The survey was approved by the Johns Hopkins Institutional Review Board and the American Society of Bone Marrow Transplantation (ASBMT). The survey was distributed by email by the ASBMT to its members on 6/27/2012 with 2 reminders sent at 2-week intervals.
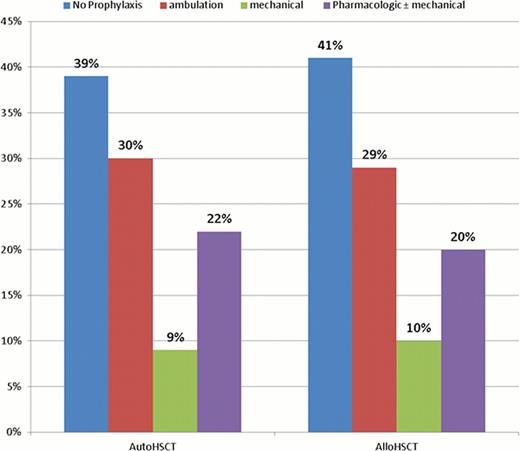
A total of 114 providers from 18 countries practicing in 95 different institutions completed the survey. The majority of responders were from the United States of America (USA) (69%); but responses were received from Canada (6); Australia (5); Mexico, Spain, Germany (3 each); India, Saudi Arabia, New Zealand (2 each); and Oman, Thailand, China, Turkey, UK, Egypt, Singapore, Chile, and Croatia (1 each). The median age of responders was 47 years (standard deviation 10.3 years), and 72% were males. Ninety-one percent of respondents were board certified in hematology or oncology. One third of responders had ≥21 years of post-fellowship experience of, while 22% were within 5 years of completing fellowship training. Fifty-six percent worked in institutions performing more than 100 HSCT annually. Forty-one percent of responders described themselves as clinicians, 46% as clinical researchers, 6% as clinical educators, and 3% laboratory researchers. The majority practiced in university-affiliated or public institutions (80%).Only 32.5% and 14% of responders worked in institutions that had cancer-specific and transplant-specific VTE prophylaxis order sets, respectively. Provider preferences for VTE prevention for patients undergoing allogeneic and autologous HSCT are displayed in Figure 1. Most respondents (79%) used a platelet count threshold of 50,000/μL for pharmacologic VTE prophylaxis. Fewer respondents used 30,000/μL (19%) or 75,000/μL as a cutoff for pharmacologic VTE prophylaxis. The primary reasons cited for the current approach to VTE prevention in HSCT patients included: 1. a perceived low risk of VTE (30%), 2. a high risk of bleeding (24%), and 3. An absence of data supporting VTE prophylaxis in HSCT patients (24%).
The first reported international web-based survey of VTE prophylaxis among health care professionals caring for HSCT patients notes considerable variation in clinical practice. These data underscore the need for further investigation to develop evidence-based recommendations for VTE prophylaxis in this vulnerable population.
VTE prophylaxis practice of 114 international providers in allogeneic HSCT (alloHSCT) and autologous HSCT (autoHSCT).
VTE prophylaxis practice of 114 international providers in allogeneic HSCT (alloHSCT) and autologous HSCT (autoHSCT).
Streiff:sanofi-aventis: Consultancy, Honoraria; BristolMyersSquibb: Research Funding; Eisai: Consultancy; Janssen Healthcare: Consultancy; Daiichi-Sankyo: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal