Abstract
Acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS) preferentially afflict patients 65 years of age and older. Patients in this age group are likely to have underlying comorbid conditions. These comorbidities affect treatment planning decisions and clinical outcomes. Here we report comorbidity-stratified outcomes of patients older than 64 treated at MD Anderson Cancer Center from 1996 until 2011, inclusive, treated with allogeneic stem cell transplant (ASCT).
182 patients older than 64 received an ASCT for AML (n=143) or MDS (n=39). Patient charts were reviewed and comorbidity data abstracted using a standardized form. Burden of comorbidity was assessed using the Hematopoetic Stem Cell Transplant-Specific Comorbidity Index (HSCT-CI). Low-risk, intermediate-risk, and high-risk patients were categorised at 0, 1–2, and >=3 points as per the HSCT-CI. 157 patients were evaluable for pre-transplant comorbidity. Outcomes of interest were cumulative incidence of transplant-related mortality (TRM), cumulative incidence of relapse-related mortality (RRM), incidence of acute and chronic graft-versus-host disease (GVHD), and overall survival (OS). These were estimated from the date of transplantation.
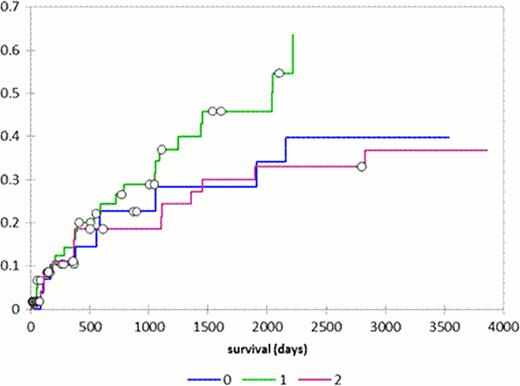
The median age of transplanted patients was 67 (range 65–79), and 37 patients age 70 and older were treated. The majority of patients were intermediate-risk and high-risk patients (table), 9 patients had HSCT-CI scores of >=5. Median follow-up for alive patients was 12.6 months (n=63; range 0–118). Cumulative incidence of TRM was 6% at 100 days, 14% at 1 year, 23% at 2 years, and 36% at 5 years (figure). Cumulative incidence of RRM was 36% at 1 year, 42% at 2 years, and 47% at 5 years. HSCT-CI did not independently predict for either TRM or RRM (log-rank test p=0.95). The incidence of grade III and IV acute GVHD was 10% of all patients. The cumulative incidence of chronic GVHD was 25% at 1 year, 27% at 2 years, and 30% at 5 years, with no association between GVHD and HSCT-CI comorbidity.
ASCT is a curative option for selected patients over age 64. HSCT-CI did not predict TRM or survival on this cohort of high-risk patients. Disease relapse was of greater concern than TRM, and so novel approaches to relapse prevention are needed.
Patient characteristics
| Category . | Parameter . | Number (%) . |
|---|---|---|
| HSCT comorbidity index | Low risk (0) | 34 (22) |
| Intermediate risk (1) | 67 (37) | |
| High Risk (2) | 56 (36) | |
| Donor type | matched related donor | 87 (48) |
| matched unrelated donor | 73 (40) | |
| mismatched unrelated donor | 17 (9) | |
| Preparative regimens | fludarabine/melphalan | 85 (47) |
| fludarabine/busulfan | 61 (34) | |
| fludarabine/idarubicin | 13 (7) | |
| Immunosuppression | tacrolimus/mini-methotrexate | 147 (81) |
| tacrolimus/mycophenolate | 8 (4) | |
| post-transplant cyclophosphamide | 16 (9) | |
| Cell source | Peripheral blood | 122 (67) |
| Marrow | 53 (29) | |
| Cord | 7 (4) | |
| Cytogenetics | Good risk | 14 (8) |
| Intermediate risk | 86 (42) | |
| Poor risk | 71 (50) | |
| Disease status at ASCT | primary induction failure | 21 (12) |
| complete remission 1 | 38 (21) | |
| complete remission 2 or 3 | 15 (8) | |
| refractory/untreated disease | 120 (66) |
| Category . | Parameter . | Number (%) . |
|---|---|---|
| HSCT comorbidity index | Low risk (0) | 34 (22) |
| Intermediate risk (1) | 67 (37) | |
| High Risk (2) | 56 (36) | |
| Donor type | matched related donor | 87 (48) |
| matched unrelated donor | 73 (40) | |
| mismatched unrelated donor | 17 (9) | |
| Preparative regimens | fludarabine/melphalan | 85 (47) |
| fludarabine/busulfan | 61 (34) | |
| fludarabine/idarubicin | 13 (7) | |
| Immunosuppression | tacrolimus/mini-methotrexate | 147 (81) |
| tacrolimus/mycophenolate | 8 (4) | |
| post-transplant cyclophosphamide | 16 (9) | |
| Cell source | Peripheral blood | 122 (67) |
| Marrow | 53 (29) | |
| Cord | 7 (4) | |
| Cytogenetics | Good risk | 14 (8) |
| Intermediate risk | 86 (42) | |
| Poor risk | 71 (50) | |
| Disease status at ASCT | primary induction failure | 21 (12) |
| complete remission 1 | 38 (21) | |
| complete remission 2 or 3 | 15 (8) | |
| refractory/untreated disease | 120 (66) |
Cumulative incidence of treatment-related mortality among HSCT-CI risk groups
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal