Abstract
We previously reported the prognostic impact of pre-transplant functional imaging (FI) on outcome following autologous stem cell transplant (ASCT) for patients with relapsed or refractory (rel/ref) Hodgkin lymphoma (HL) (Moskowitz AJ, et al. Blood 2010). This analysis was based upon patients treated on 3 consecutive Memorial Sloan-Kettering Cancer Center (MSKCC) clinical trials from 1994 to 2003. The cohort included patients evaluated by gallium or FDG-PET and the 5 year event free survival (EFS) for patients with normal vs abnormal pre-transplant FI was 75% and 31% respectively. Based upon these results, our treatment program has focused on the use of FDG-PET to determine eligibility for ASCT. While determination of FI results in our series was based upon visual interpretation, we now aim to investigate whether semi-quantitative evaluation of pre-transplant FDG-PET could better distinguish favorable and less favorable cohorts.
Patients with rel/ref HL treated on MSKCC clinical trials who underwent pre-salvage and pre-transplant evaluation with FDG-PET were included in this analysis. Pre-salvage and pre-transplant FDG-PET reports were reviewed and maximum SUV values for each scan were recorded. The delta-SUV was a calculation of the percent change in maximum SUV between pre-salvage and pre-transplant FDG-PET. EFS was calculated using the Kaplan-Meier method. The prognostic impact of FDG-PET results by visual interpretation and semi-quantitative interpretation was evaluated using the log-rank test.
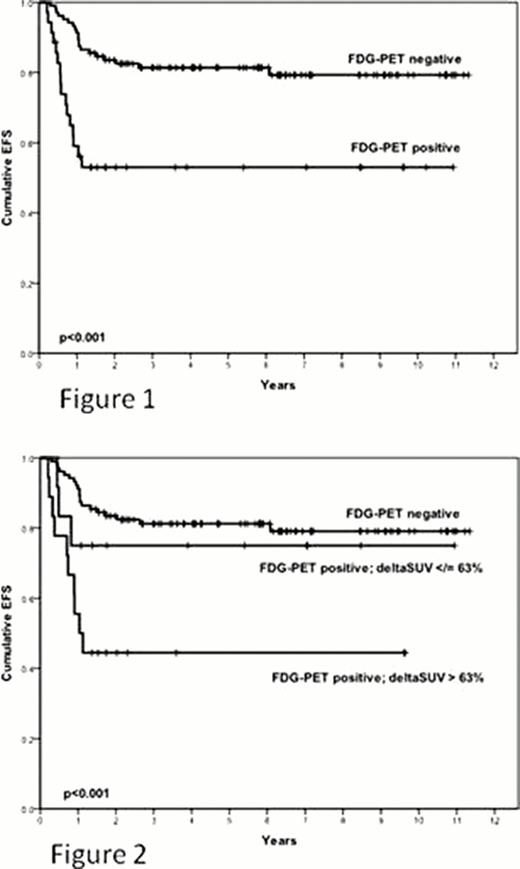
One hundred and thirty nine patients with rel/ref HL treated on consecutive MSKCC clinical trials from October 2000 through August 2010 were evaluated. Of the 139 patients, 104 (75%) achieved FDG-PET normalization prior to ASCT. The median follow-up for survivors was 6 years. The 6 year EFS for FDG-PET negative and FDG-PET positive patients was 79% and 53% respectively (p<0.001, figure 1). Among the patients with abnormal pre-transplant FDG-PET, the median maximum SUV value was 4.3 and the median delta-SUV was 60%. We tested absolute pre-transplant maximum SUV values of 2, 3, 4, and 5 and we were unable to find a value of prognostic significance among FDG-PET positive patients. We tested delta-SUV values of 50%, 60%, 63%, 66%, and 72.9%. Patients with positive pre-transplant FDG-PET and ≥63% delta-SUV were found to have similar outcomes as patients with negative pre-transplant FDG-PET (p=.47, figure 2). The 6 year EFS for delta-SUV ≥63% patients was 77% compared to 44% for delta-SUV < 63% (p=0.12).
For rel/ref HL patients undergoing ASCT, semi-quantitative evaluation of pre-transplant FDG-PET using delta-SUV of 63% identifies a favorable cohort among patients with positive pre-transplant FDG-PET. The difference in outcome for patients with ≥63% delta-SUV and < 63% delta-SUV was not statistically significant, however, likely due to the small number of FDG-PET positive patients in our series. Nevertheless, patients who achieve delta-SUV of at least 63% prior to ASCT achieved similar outcomes as those with negative pre-transplant FDG-PET. The prognostic significance of the 63% delta-SUV cutoff needs to be evaluated further in prospective studies.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal