Abstract
Abstract 1993
Recent advance in allogeneic hematopoietic stem cell transplantation (HSCT) has led to an increasing use of transplantation for older, having comorbidities, and more heavily pretreated patients. Thus, the evaluation of comorbidity is of increasing importance in order to estimate precisely benefits and risks of transplant procedure. The HCT-CI scoring system has been proposed, and has been confirmed as a useful tool to predict the probability of post-transplant non-relapse mortality (NRM) and overall survival (OS) while taking into account any pre-transplant comorbidity. However, HCT-CI has not been fully validated by prospective studies in multicenter setting, and its predictive value remains to be elucidated in Japanese population.
The aim of this cohort study is to prospectively evaluate whether HCT-CI score could be predictive for transplant outcomes Japanese patients in multicenter transplant setting.
244 consecutive patients (median age 45.3 years; range 16 to 74) with a variety of hematological disorders who had received myeloablative (MA, n= 167) or reduced-intensity (RIST, n= 77) conditioning followed by the first HSCT were enrolled in this study from 2007 to 2009 in 14 facilities of the KSGCT in Japan. The stem cell sources included bone marrow (BM, n=156), peripheral blood (PB, n=30) and cord blood (CB, n=58). The commonest diagnosis was myeloid malignancies (AML/MDS; 58.2 %) followed by ALL (18.4%), and NHL (10.7%). Pre-transplant co-morbidities were scored according to original HCT-CI scoring system in all patients. Patients were followed for 2 years or until relapse/death before two years after transplantation.
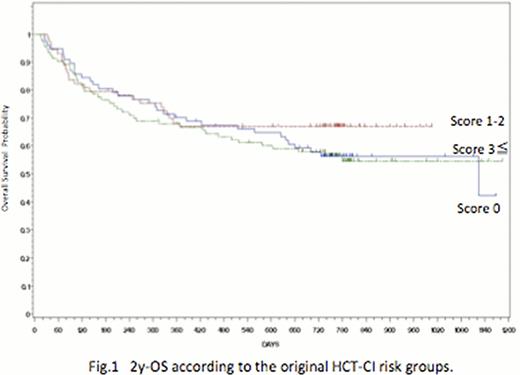
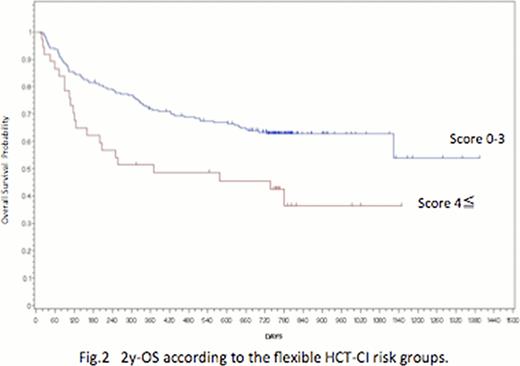
The most frequent comorbidity observed was mild & severe pulmonary comorbidities (51.9%), followed by mild hepatic comorbidity (14.6%) and active infections (9.3%). The other comorbidities observed in this cohort included psychiatric problems (4.8%), diabetes (3.6%), moderate to severe hepatic (2.8%), and solid tumors (2.8%). The OS and NRM of all patients were 59.2% and 20.4% at 2 years, respectively. The proportion of patients with HCT-CI score 0, 1–2, 3≤ was 32%, 30%, 38%, respectively. The original HCT-CI score failed to predict for OS and NRM (Fig 1). Furthermore, it was not correlated with KS score at 2Y and specific causes of death. We then applied flexible HCT-CI risk scoring system (re-stratified as low-risk; 0–3, and high-risk; 4≤). The distribution of flexible HCT-CI score did not differ significantly in terms of age at the time of transplant (51≤ vs. ≤50), sources of stem cells (BM vs. PB vs. CB), and conditioning (MA vs. RIST). The better predictive capacity for NRM and OS at 2Y of the flexible HCT-CI than original HCT-CI was confirmed (p=0.003) (fig 2). Multivariate analysis identified age (≥50) (p=0.010, HR=1.80), PS (≥90%) (p=0.010, HR=2.57), donor type (HLA-mismatched/unrelated donor) (p=0.020, HR=1.82), and flexible HCT-CI score (4≤) (p=0.019,HR=1.82) as significant predictors of worse OS at 2Y. However, flexible HCT-CI score did not remain as significant predictor of NRM at 2Y while age (p=0.017, HR=2.17), PS (p=0.0001, HR =4.60)and donor type (p =0.019, HR=2.80) remained as significant predictors.
Our multicenter prospective study suggests that the modified 2-group scoring HCT-CI, not the original scoring HCT-CI, is a useful predictor of 2 -year OS but not NRM in Japanese. Reconsidering the scoring weight of comorbidity and incorporation of other risk factors (age, PS and donor type) may further improve the predictive capacity of flexible HCT-CI scoring system.
Nannya:Otsuka Seiyaku Koujyou: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal