Abstract
Abstract 1989
High-dose chemotherapy followed by autologous stem cell transplant can improve long-term outcome of patients with hematologic malignancies. Outcomes following transplant are variable. Obesity has implications for stem cell mobilization, chemotherapy administration, and medication dosing. We analyze the impact of obesity on transplant outcomes including neutrophil recovery, platelet recovery, length of hospital stay, and survival.
From 1/2004 to 12/2009, 573 patients underwent autologous stem cell transplant. From these patients, 17 were excluded due to incomplete data. Of the remaining 556 patients, the median age was 53 years, and 346 (62%) were male. The diagnoses were 286 (51%) non-Hodgkin lymphoma, 161 (29%) multiple myeloma, 91 (16%) Hodgkin lymphoma, and 18 (3.2%) other. A majority of these patients (93%) had received 3 or less prior chemotherapy regimens. Most patients (76%) had not received prior radiation therapy. Most patients had chemosensitive disease (92% were in complete or partial remission) at time of transplant. For stem cell mobilization regimen, 376 (68%) received chemotherapy and G-CSF, 176 (32%) received G-CSF alone, and 4 (<1%) received G-CSF and Plerixafor. For a preparative regimen, 360 (65%) received busuflan/etoposide/cyclophosphamide, 125 (23%) received melphalan, and 71 (13%) received busulfan/cyclophosphamide.
Patients were categorized into four groups based on the body mass index (BMI): underweight (BMI<18.5), normal (18.5–24.9), overweight (25.0–29.9), or obese (≥30.0). Using these definitions, there were 5 (1%) underweight, 133 (24%) normal, 188 (34%) overweight, and 230 (41%) obese patients. Underweight and normal were combined into a single group due to the small number of underweight patients. Baseline and transplant characteristics of these patients are listed in Table 1. Variables were compared among BMI groups using the Chi-square test (categorical variables), Kruskal-Wallis test (continuous variables), or log-rank test (survival). Cox proportional hazards analysis was used to identify prognostic factors for survival.
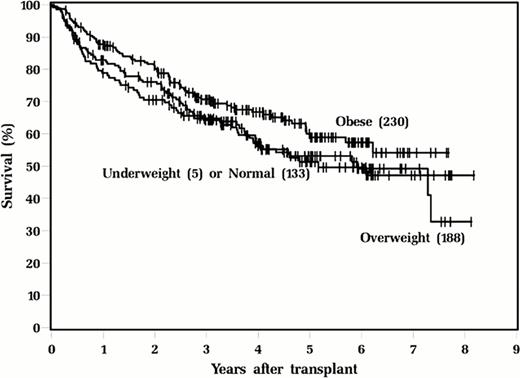
On univariable and multivariable analyses, obese patients demonstrate better survival than those who are not obese (hazard ratio 0.73, P=0.026; Figure 1).
In conclusion, obesity has no impact on neutrophil or platelet recovery, length of transplant hospitalization, or 100-day mortality. Obese patients appear to have improved overall survival. The reasons for this are unclear, but may have to do with higher total dose of chemotherapy for the preparative regimen. Although obesity is associated with many co morbidities and possibly more aggressive disease, these patients do not have cancer cachexia and may have other protective benefits.
Patient and transplant characteristics according to BMI
| . | Underweight/ Normal N = 138 . | Overweight N = 188 . | Obese N = 230 . | . |
|---|---|---|---|---|
| Variable | N (%) | N (%) | N (%) | P-value |
| Gender | ||||
| Male | 63 (46) | 136 (72) | 147 (64) | <0.001 |
| Female | 75 (54) | 52 (28) | 83 (36) | |
| Age, years | ||||
| Median (range) | 50 (20–74) | 55 (20–73) | 54 (19–75) | 0.013 |
| Number of prior chemotherapy regimens | ||||
| ≤ 3 | 130 (94) | 177 (94) | 212 (92) | 0.65 |
| >3 | 8 (6) | 11 (6) | 18 (8) | |
| Prior radiation therapy | ||||
| Yes | 38 (28) | 45 (24) | 53 (23) | 0.61 |
| No | 100 (72) | 143 (76) | 177 (77) | |
| Diagnosis | ||||
| NHL | 74 (54) | 98 (52) | 114 (50) | 0.025 |
| MM | 28 (20) | 53 (28) | 80 (35) | |
| HL | 33 (24) | 30 (16) | 28 (12) | |
| Other | 3 (2) | 7 (4) | 8 (4) | |
| Disease status at transplant | ||||
| CR/PR | 120 (87) | 172 (91) | 217 (94) | 0.048 |
| Active disease | 18 (13) | 16 (9) | 13 (6) | |
| Mobilizing regimen | ||||
| G-CSF+chemotherapy | 106 (77) | 126 (67) | 144 (63) | 0.05 |
| G-CSF alone | 32 (23) | 61 (32) | 83 (36) | |
| G-CSF + Plerixafor | 0 (0) | 1 (0.5) | 3 (1) | |
| Preparative regimen | ||||
| Bu/VP/Cy | 94 (68) | 128 (68) | 138 (60) | 0.22 |
| Melphalan | 30 (21) | 34 (18) | 61 (27) | |
| Bu/Cy | 14 (10) | 26 (14) | 31 (13) | |
| CD34+ dose, × 106/kg | ||||
| Median (range) | 6.19 (2.11–47.97) | 5.67 (2.06–65.18) | 7.01 (1.62–51.90) | 0.21 |
| Days to ANC > 500 | ||||
| Median (range) | 11 (9–13) | 11 (9–17) | 10 (9–15) | 0.36 |
| Days to platelet > 20,000 | ||||
| Median (range) | 14 (6–129) | 14 (5–432) | 14 (3–46) | 0.48 |
| Length of hospital stay | ||||
| Median (range) | 21 (13–30) | 20 (13–74) | 20 (12–37) | 0.08 |
| 100-day mortality | ||||
| Yes | 9 (7) | 9 (5) | 4 (2) | 0.06 |
| No | 129 (93) | 179 (95) | 226 (98) |
| . | Underweight/ Normal N = 138 . | Overweight N = 188 . | Obese N = 230 . | . |
|---|---|---|---|---|
| Variable | N (%) | N (%) | N (%) | P-value |
| Gender | ||||
| Male | 63 (46) | 136 (72) | 147 (64) | <0.001 |
| Female | 75 (54) | 52 (28) | 83 (36) | |
| Age, years | ||||
| Median (range) | 50 (20–74) | 55 (20–73) | 54 (19–75) | 0.013 |
| Number of prior chemotherapy regimens | ||||
| ≤ 3 | 130 (94) | 177 (94) | 212 (92) | 0.65 |
| >3 | 8 (6) | 11 (6) | 18 (8) | |
| Prior radiation therapy | ||||
| Yes | 38 (28) | 45 (24) | 53 (23) | 0.61 |
| No | 100 (72) | 143 (76) | 177 (77) | |
| Diagnosis | ||||
| NHL | 74 (54) | 98 (52) | 114 (50) | 0.025 |
| MM | 28 (20) | 53 (28) | 80 (35) | |
| HL | 33 (24) | 30 (16) | 28 (12) | |
| Other | 3 (2) | 7 (4) | 8 (4) | |
| Disease status at transplant | ||||
| CR/PR | 120 (87) | 172 (91) | 217 (94) | 0.048 |
| Active disease | 18 (13) | 16 (9) | 13 (6) | |
| Mobilizing regimen | ||||
| G-CSF+chemotherapy | 106 (77) | 126 (67) | 144 (63) | 0.05 |
| G-CSF alone | 32 (23) | 61 (32) | 83 (36) | |
| G-CSF + Plerixafor | 0 (0) | 1 (0.5) | 3 (1) | |
| Preparative regimen | ||||
| Bu/VP/Cy | 94 (68) | 128 (68) | 138 (60) | 0.22 |
| Melphalan | 30 (21) | 34 (18) | 61 (27) | |
| Bu/Cy | 14 (10) | 26 (14) | 31 (13) | |
| CD34+ dose, × 106/kg | ||||
| Median (range) | 6.19 (2.11–47.97) | 5.67 (2.06–65.18) | 7.01 (1.62–51.90) | 0.21 |
| Days to ANC > 500 | ||||
| Median (range) | 11 (9–13) | 11 (9–17) | 10 (9–15) | 0.36 |
| Days to platelet > 20,000 | ||||
| Median (range) | 14 (6–129) | 14 (5–432) | 14 (3–46) | 0.48 |
| Length of hospital stay | ||||
| Median (range) | 21 (13–30) | 20 (13–74) | 20 (12–37) | 0.08 |
| 100-day mortality | ||||
| Yes | 9 (7) | 9 (5) | 4 (2) | 0.06 |
| No | 129 (93) | 179 (95) | 226 (98) |
Survival outcomes according to BMI
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal