Abstract
High dose chemotherapy followed by autologous stem cell transplantation (ASCT) remains the standard of care for patients with relapsed or refractory (R/R) diffuse large B cell lymphoma (DLBCL) who are chemosensitive to salvage therapy. There is now evidence that the achievement of complete remission by PET scan (PET-CR) after salvage therapy is a favorable determinant of ASCT outcome, implying that PET response should be part of the prognostic assessment for patients considering ASCT. However, it is unclear whether other prognostic factors are still relevant in patients getting post-salvage PET scanning. Moreover, while ASCT is often also used for patients with R/R transformed indolent lymphoma (TIL), there are no data on whether prognostic factors that are important for DLBCL patients, especially PET response to salvage, are similarly prognostic in this population.
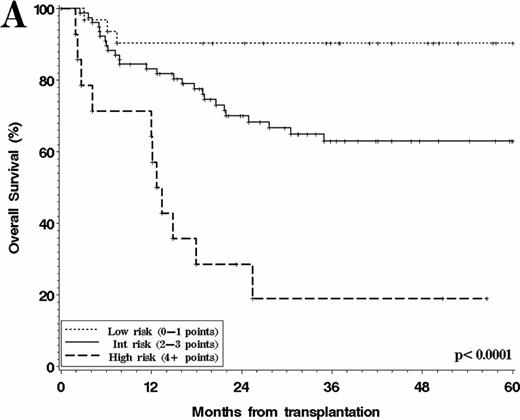
We studied 163 consecutive adult patients who underwent ASCT at 2 institutions over the last decade for R/R DLBCL (122 patients) or R/R TIL (41 patients) and had a post-salvage PET scan. 98% were chemosensitive after salvage by conventional criteria. Among the 122 patients with DLBCL, 52 (43%) remained PET positive after salvage. PET-positivity was more likely for patients with advanced stage at relapse, and for those whose first remission duration was less than 6 months. After a median follow-up of 49 months from ASCT, the 4-year overall survival (OS) for PET-positive patients was 54% versus 74% for PET-negative patients (p=0.016), while the corresponding 4-year progression-free survival (PFS) was 30% versus 63% (p<0.0001). In multivariable models, the following were adverse prognostic factors for OS and PFS: PET positivity after salvage, age ≥60 years, CNS involvement at relapse, symptomatic relapse, and advanced stage at relapse (for OS only). Based on those factors, we constructed a prognostic score, assigning 1 point for each of the above factors (except for CNS relapse which was assigned 3 points). Patients in the low-risk group (0–1 points) had a 4y OS of 90% and 4y PFS of 74%, compared to 63% and 45% for patients in the intermediate-risk group (2–3 points), and 19% and 0% for patients in the high-risk group (4+ points) (p<0.0001 for both OS and PFS differences) (Figure 1A).
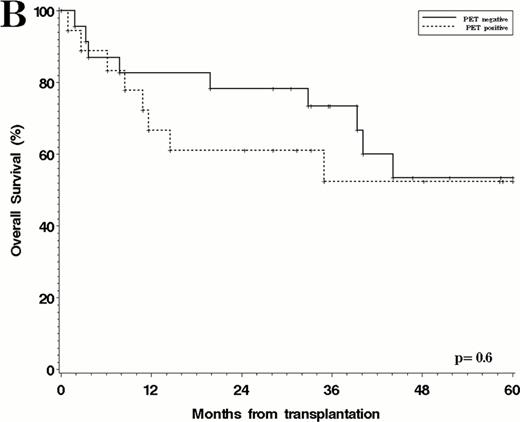
The post-ASCT outcome of patients with TIL was not significantly different from that of DLBCL patients (4y OS 53% versus 69%, p=0.23, and 4y PFS 44% versus 54%, p=0.4). Notably, in this group, PET status after salvage had no prognostic relevance (Figure 1B). In fact, in multivariable models for OS and PFS, only short duration of 1st remission and elevated LDH at relapse (for OS only) were significant.
Overall Survival after ASCT. A. DLBCL cohort, stratified by prognostic score; B. TIL cohort, stratified by post-salvage PET.
Overall Survival after ASCT. A. DLBCL cohort, stratified by prognostic score; B. TIL cohort, stratified by post-salvage PET.
This study confirms the prognostic importance of post-salvage PET remission status. However, If PET response is included in the prognostic assessment, traditional risk factors such as receipt of 1st line rituximab, short duration of 1st remission, or elevated second-line aaIPI appear to lose their prognostic importance. Instead, we identified 4 other clinical factors that were strongly associated with outcome: advanced age, CNS relapse, advanced stage at relapse, and symptomatic relapse. Our prognostic score is simple to calculate and stratifies patients into 3 groups with significantly different OS and PFS. An important potential use of this score, if further validated, could be to identify a high-risk population whose outcomes after ASCT are dismal (0% PFS and 19% OS at 4 years), and who should be considered for alternative treatment approaches. Moreover, our results suggest that prognostic factors for patients with TIL may be entirely different; in particular, PET response to salvage may not be prognostically important. This is important to consider when designing clinical trials or interpreting their results in this patient population.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal