Abstract
17p- is a principle predictor of poor outcome in CLL patients after conventional chemotherapy. Since 2007, the MD Anderson Leukemia Service initiated a concerted effort to refer CLL17p- patients for NST consideration at the time of their first presentation. While studies have suggested NST to be able to overcome this adverse prognostic impact, the applicability of this NST for the majority of patients and potential selection bias remains unclear.
We retrospectively reviewed outcomes of CLL 17p- patients to determine how often patients underwent NST(NST+), the reasons they did not (NST-), and whether any characteristics, including survival, differed between the two groups.
52 CLL17p- patients were referred to the Transplant Service between 2007–2010. Wilcoxon rank-sum and Fisher's exact tests were used to compare clinical variables of interest by NST status. Kaplan-Meier survival curves and Cox proportional hazards regression were used to estimate survival.
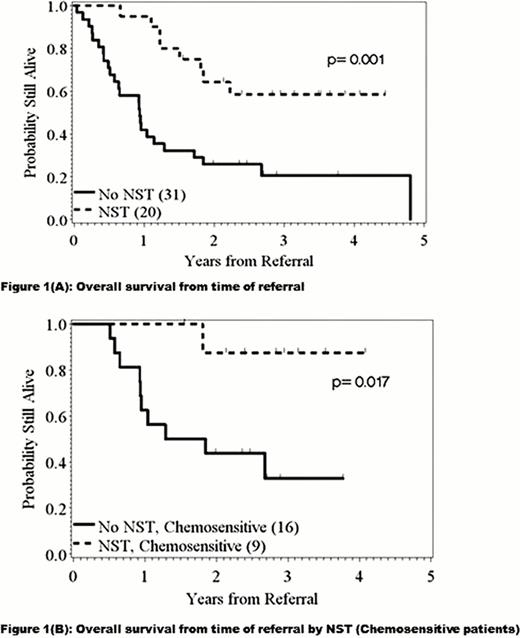
20 (38%) of the 52 referred patients underwent NST. The remaining 32 patients (62%) were not transplanted for the following reasons: death due to pre-NST salvage treatment/or disease related complications (n=15, 47%); physician/patient preference in chemosensitive patients (n=10, 31%); lost to follow up (n=4, 12.5%); no available donors (n=3, 9%). 21(40%) were previously untreated, while 31 (60%) had received a median of 4 lines of treatments at other centers. No significant difference was observed in age at referral between the two groups (median 54 years for NST+ vs 60 years for NST-, p=0.2). In addition, no significant differences were observed for several other patient characteristics, including gender, beta2-microglobulin, associated myelodysplasia, number of prior treatments, ZAP-70+, unmutated heavy chain, or presence of additional cytogenetic abnormalities. Although more patients in the NST- group had elevated lactate dehydrogenase level than in the NST+ group (84% vs 45%, p= 0.0049), there was no significant difference observed in documented Richter's (25% vs 15%, p=0.5). Median follow up from the time of diagnosis and referral was 5.3 years (range 0.7–22 years) and 1.5 years (range 0.1–4.8 years) respectively. The 2-year post-referral PFS rates were 50% and 8% in the NST+ and NST- groups, respectively. 2-year post-referral OS rates were 64% and 25%, respectively (Fig 1A). More importantly, the OS benefit for the NST+ group remained significant even when analysis was restricted to the chemosensitive patients who received NST and those with chemosensitive disease who opted, per patient or physician preference, not to receive NST. The 2-year OS rates for the two groups were 88% and 43%, respectively (Fig 1B). Treatment-related mortality in the NST+ group was 21% at 1-year. Significant univariate determinants of PFS following NST included refractory disease status (p=0.043), number of prior chemotherapies (0.045), and lymph node size >5 cm (p=0.010) at the time of transplant. Lymph node size >5 cm (p=0.031), number of prior therapies (p=0.019), age at transplant (p=0.047), beta-2 microglobulin >4 mg/L (p=0.016), and CD34+ infused (p=0.022) were significant predictors of OS. There was a strong correlation between beta-2 microglobulin level and lymph node size (Spearman rho=0.68, p=0.0018). Multivariate analysis could not be performed due to the sample size.
Our study demonstrates that for CLL 17p- patients, allogeneic NST has been associated with a superior outcome to conventional chemotherapy even amongst patients with chemosensitive disease. Our findings provide rationale for consideration of NST in the upfront setting for this subset of patients.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal