Abstract
Abstract 1948
Previous studies on the reconstitution of regulatory T cells (Treg) after allogeneic hematopoietic stem cell transplantation (HSCT) have shown a delayed reconstitution in patients (pts) with acute graft-versus-host-disease (GvHD) (Magenau, 2010) and an association between impaired Treg reconstitution and the development of extensive chronic GvHD (Matsuoka, 2010). However, no studies have analyzed naive (nTreg) versus memory (mTreg) Treg reconstitution in a longitudinal cohort with large numbers of pts.
From 2006 to 2009, 165 consecutive pts were prospectively analyzed in our center post-HSCT. Fresh whole blood samples were obtained 3 (n=155), 6 (n=162), 12 (n=165) and 24 (n=94) months after HSCT and analyzed by flow cytometry to quantify CD4 T cells, including naive, activated, central memory and effector memory subsets (Sallusto, 1999), as well as Treg (CD4+ CD25+ CD127neg/lo), including nTreg (CD45RA+) and mTreg (CD45RAneg). The results are presented as median values of circulating cells. Median age was 41 years (range: 6–68). The indication for HSCT was malignant disease in 92%. The conditioning regimen was reduced-intensity (RIC) in 51%. The donor was an HLA-identical sibling in 56%. The source of stem cells was peripheral blood (PBSC), bone marrow (BM) and cord blood (CB) in 65%, 28% and 7%, respectively. All pts received cyclosporine as GvHD prophylaxis. GvHD was defined as acute if occurring before day 100 and chronic thereafter.
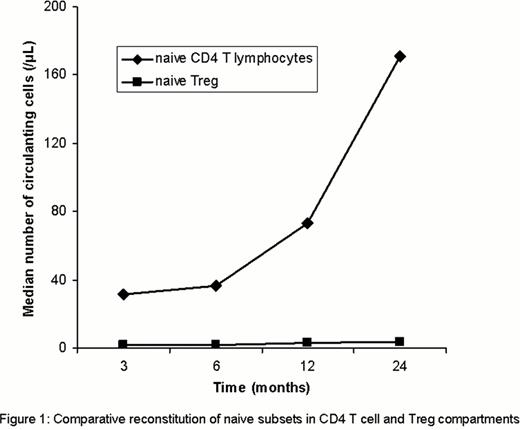
Total Treg (tTreg) increased from 13/μL at 3 months to 44/μL at 24 months, but always remained inferior to healthy controls (HC) (66/μL). nTreg increased from 1.8/μL at 3 months to 4.8/μL at 24 months (HC: 24/μL). mTreg increased from 10.7/μL at 3 months to 33.3/μL at 24 months (HC: 42/μL). The CD4/Treg ratio remained stable at 12.6 at 3 months and 11.6 at 24 months while the nCD4/nTreg ratio increased from 17.4 at 3 months to 42.7 at 24 months, showing a larger expansion of naive cells in the CD4 T cell compartment than in the Treg compartment (Figure 1) and a larger expansion of memory cells in the Treg than within the CD4 cells. At 3 months post-HSCT, tTreg, nTreg and mTreg were significantly higher in PBSC recipients (18.4, 2.7 and 14.5/μL) than in BM (8.1, 0.9 and 6.5/μL) and CB recipients (6.5, 0.6 and 5.3/μL) (p=0.0001), respectively. Pts transplanted after a RIC regimen had significantly more tTreg and mTreg than pts transplanted after a standard regimen (17 and 14/μL, compared with 9.8 and 8/μL, p=0.004 and 0.008 respectively). Pts transplanted for an aplastic anemia had significantly fewer nTreg than pts transplanted for a malignant disease (0.4 and 1.9/μL, p=0.001). At 6 months post-HSCT, tTreg, nTreg and mTreg were significantly higher (p=≤0.01) in pts transplanted from an HLA-identical sibling (19.5, 1.9 and 17.2/μL) compared with pts transplanted from an unrelated donor (13.2, 1.2 and 11/μL). At 12 and 24 months post-HSCT, younger pts (≤15 years) had significantly more nTreg than older pts (9.8 and 28.7/μL compared with 2.1 and 4.2, p=0.001). In pts with previous acute GvHD, tTreg and mTreg were significantly lower at 3 (8.5 and 7.7/μL) and 6 months (14.6 and 12.5/μL) compared with pts without (15.6 and 13.8/μL at 3 months, p=0.005 and 21.3 and 18.2/μL at 6 months, p≤0.007), respectively. Absolute numbers of tTreg, nTreg and mTreg, and the frequencies of Treg relative to activated, effector memory and central memory CD4 T cells at 3, 6 and 12 months post-HSCT did not predict the occurrence of a later episode of chronic GvHD up to 2 years post-HSCT.
In our population, total, naive and memory Treg reconstitution was delayed post-HSCT and remained below the normal range up to 2 years after HSCT. tTreg reconstitution post-HSCT was mostly due to mTreg expansion. RIC regimen and PBSC as source of stem cells were associated with a better short-term reconstitution. At 6 months, pts transplanted from siblings had a better reconstitution while nTreg long-term reconstitution was mainly influenced by recipient age (better if ≤15 years). While previous acute GvHD impaired Treg reconstitution, Treg subsets (absolute numbers and frequencies relative to CD4 T cell subsets) at 3, 6 and 12 months post-HSCT were unable to predict chronic GvHD in this large cohort of patients. We believe these data are of particular interest regarding the recently increasing number of Treg interventional studies in humans in the context of HSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal